Date: 3 May 2013
Yamik catheter for rinsing nasal and paranasal cavities. Image C
Copyright:
These images were kindly given by Andreas Neher of the Department of Otorhinolaryngology, Innsbruck Medical University, Anichstr. 35, Innsbruck, Austria. For further details of the procedure please refer to the PDF link above. (C) Fungal Research Trust
Notes:
Rinsing of the nasal and paranasal cavities applied via a novel catheter system (YAMIK). The cavities were rinsed with 10–20 ml of 1% aqueous N-Chlorotaurine (NCT) solution, treatment consisted of three lavages per week for 4 weeks. N-Chlorotaurine is a mild endogenous oxidant with broad-spectrum antimicrobial activity. The use of the catheter proved to be a successful way of rinsing the nasal and paranasal cavities. Link to PDF with further details.
C,D X-ray set up of a healthy volunteer rinsed with 10 ml of radio-opaque solution via YAMIK catheter demonstrating sufficient filling of the paranasal sinuses.
Images library
-
Title
Legend
-
PtDS2 –Repeated chest infections arrested by itraconazole therapy in ABPA and bronchiectasis
DS2 developed asthma age 24 and now aged 62. From about age 30 she started getting repeated chest infections and a few years later ABPA and bronchiectasis was diagnosed. Infections continued requiring multiple courses of antibiotics annually. At one point DS2 developed a pneumothorax, possibly because of excess coughing. She has chronic rhinitis and mannose binding lectin deficiency. In May 2011, she started itraconazole therapy, and has needed no antibiotic courses for her chest since. Her rhinitis with sinusitis occasionally bothers her. She is delighted to have gone 18 months with no chest infections.
 ,
,  ,
, 
-
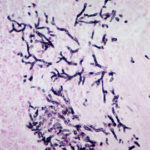
Aspergillus hyphae (arrow) in the lumen without invasion of the necrotic bronchial wall (*) (Nicod 2001).
-
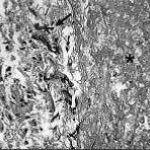
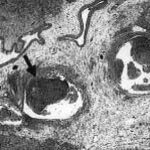
fibrinonecrotic material (arrow) from the airway shown in A, with subocclusion of the bronchial lumen (*)
-
Fibrinous or pseudomembranous bronchitis (arrow) with subocclusion of the airways (* indicates subocclusion of the airways by pseudomembranes)

-
Bronchoscopic biopsy demonstrated septate hyphae with branching at 45o (methenamine silver stain ×400).