Air quality is fundamentally important to our health. If the air that we breathe contains particular pollutants it can trigger medical problems, including asthma attacks and heart attacks. Pollutants can be found in the form of gasses, vapours and particulates: all are capable of penetrating deep into our lungs to sensitive tissues. Once in our lungs, they can irritate and (in some cases) penetrate the thin linings of our lungs. These are designed to allow gasses to pass through into our bloodstream, rather than protect us from toxins.
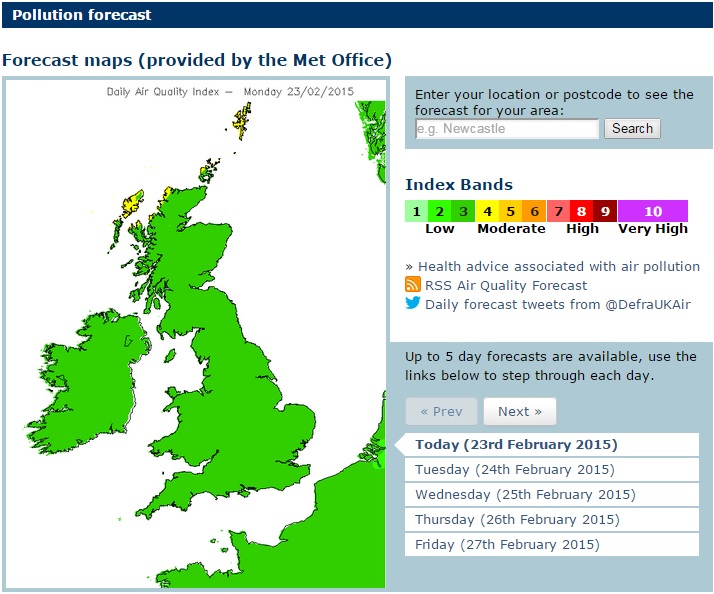
Interested readers can read about the threats of air pollution on the UK government DEFRA website. Here, it is possible to access real time data on air pollutants taken at multiple monitoring sites throughout the UK. A committee of medical experts (Committee on the Medical Effects of Air Pollutants — COMEAP) advises the UK government on the health implications of the measured levels of air pollutants. The most common harmful air pollutants are classified into the following categories:
• Nitrogen Dioxide
• Sulphur Dioxide
• Carbon Monoxide
• Ozone
• Particles < 2.5µm (PM2.5) and Particles < 10µm (PM10)
Air Pollution – Moulds
Moulds such as Aspergillus and Penicillium are frequently found suspended in the air. This diagram (taken from the Midlands Asthma & Allergy Research Association website — MAARA) shows how different types of moulds and fungi proliferate at different times of the year in warm temperate areas, such as the UK. However, they all tend to peak in the period from June to August.
Counts taken by MAARA show that fungal spores in the air exceeded 50,000 spores per cubic metre of air during this time — mainly Cladosporium, Sporobolomyces and Basidiospores, but also Aspergillus/Penicillium and Alternaria spores. This can far exceed the numbers of pollen grains in the same amount of air.
Analysis of airborne spores’ impact on our health is complicated, as plant pollens are also plentiful at these times of the year. Hayfever is probably the predominant allergy noted at these times but people can also be allergic to each of the fungal spores. The symptoms are similar (sore eyes, runny nose, skin rashes) so it is difficult to know if you are suffering from hay (pollen) allergy or allergy to fungi — medical tests are often necessary to distinguish the two.
Fungal spores (2-30 micrometers) tend to be far smaller than pollen grains (10-100 micrometers) and this has an important influence on their pathogenicity. Aspergillus spores can be 2-3 micrometer in diameter which enables them to penetrate deep into our lungs, even as far as individual alveoli. As a consequence, pollen tends to cause symptoms in our sinuses and upper airways, while fungal spores can affect our lower respiratory tract. Fungal spores are also ‘seeds’ for the growth of entire fungal colonies and thus, once they manage to get a foothold in our lungs, they can grow and be very difficult to eradicate. In contrast, pollen grains have a very limited lifespan as they are only intended to grow a short way into a flower before they die!
Indoor air – Moulds
Some estimates find that, on average, we spend 80-90% of our time indoors. The quality of our indoor air is therefore likely to be very important to our health. We know that outdoor air fundamentally influences indoor air with respect to the levels of microbes and allergens, so we can expect allergy symptoms continue indoors. This is unsurprising, as our homes are not completely airtight (even with all of our windows and doors shut). Even very small cracks and gaps seem to be sufficient to allow spores into our homes in large numbers. Additionally, it is in the summer months, when spore levels are at their highest, that we are likely to have more windows open to let air in.

However, indoors our air can be much less ‘fresh’ — i.e. the amount of air exchange between outside and inside can be low. In many countries throughout the world, people still cook over open or poorly-ventilated fires. The smoke released into the home is highly dangerous, causing widespread lung disease.
In wealthier countries, since the 1970s there has been a drive to conserve energy within homes. In the UK this was achieved by reducing the ways in which our homes lose heat — i.e. by filling our walls and roof spaces with insulation, and draught-proofing by installing sealed doors and double-glazed window units. Open fires have also been removed and replaced with gas or electrical fires, while old chimneys have been blocked up and often sealed. Homes have become warmer but also much more airtight.
At the same time, our living habits have led to us washing much more clothing, and often drying it indoors. We also bathe or shower daily rather than weekly. Water consumption has therefore risen significantly since the 1970s.
The net effect of these changes is that, although our homes are warmer, they are more prone to damp. Warmer air can hold more moisture, which is then released as the air cools (e.g. at night when heating is lower). This is a particular problem in colder weather as walls and windows become colder. Damp is a requirement for mould growth — the prevention of damp often requires specialist advice and is a result of both occupant habits and building structure/management.
Health Effects – Moulds
Many people are vulnerable to developing allergies in ways we do not yet fully understand. For the most part they seem to follow prolonged exposure to a particular allergen — for example, breathing in moulds and other substances that have proliferated in damp buildings.
Allergic Fungal Infection
Allergic fungal infections affect the upper or lower respiratory tract (although in a sense all allergies are generalised). There can also be an inflammatory component to some skin and mucosal fungal infections. However, this is not usually driven predominantly by IgE, eosinophils, mast cells and basophils: the key features of allergic disease. Many allergies are mild and have a minor effect on health. This section focuses on those that have a major impact on health.
Rarely is a person only allergic to one or more fungi: typically, those affected have a number of coexisting allergies. Additionally some disease states, such as HIV infection or cystic fibrosis, can increase the rate of allergies. However, this only appears to be relevant for fungal infection in terms of Aspergillus allergy in cystic fibrosis.
An allergic tendency (or atopy) is often apparent early in life, but can change with age. For example, many children with asthma ‘grow out of it’, although some develop it again as they get older. The long term natural history of fungal allergy is not well documented. Some people have allergic fungal infection that comes and goes in severity, usually for unclear reasons. Mucus production and mucosal swelling in the airways, nose and sinuses is the hallmark of fungal allergy. Most allergic fungal infection probably has an important genetic component.
Important allergic fungal infections include:

Chronic fungal infection
Evidence is starting to emerge that some people — possible several hundred thousand people in the UK — are vulnerable to deep fungal infections, mostly of the lungs. There are several hundred known cases in the UK, but true numbers are probably higher as diagnosis is uncommon and difficult. Some speculate that there is a continuum of infection starting with SAFS, moving to ABPA, and finally progressing to chronic pulmonary aspergillosis.
Certain groups are vulnerable because of pre-existing damage to their lungs — for instance, those who have had TB, or those with Cystic Fibrosis or COPD. Genetic research on people with ABPA is starting to reveal consistent genetic features in those who progress to chronic infection. This renders them slightly less able to rapidly fight off fungal infection, allowing the fungus gain a foothold and begin to grow. These patients do not acquire an invasive infection as their lungs can still fight off the infecting mould, but they do generally end up with a long-term, incurable, debilitating and very slow-growing infection.

It might be appropriate to assume that if someone from these vulnerable groups were to be exposed to higher levels of fungal spores in the air, they could run a higher risk of infection compared with the rest of the population. At the moment there is no way to screen for people with many of these genetic differences. However, this is a primary aim of the research being undertaken.
Some fungi are persistent, defying treatment and leading to long-term infection. In most cases, local trauma or damage is a key risk factor, including damage to the cornea of the eye (fungal keratitis) or skin inoculation of a particular fungus (such as those causing mycetoma). Prior lung disease is a major risk factor for chronic pulmonary aspergillosis, but it is not known if the same is true for chronic infection of the sinuses. Although we have included fungal keratitis and fungal sinusitis in this section, it should be noted that not all patients in these categories are immunocompromised, unlike those with invasive fungal infections.
For more information on the most common chronic and destructive Aspergillus fungal infections:
Invasive Aspergillosis
This group of fungal infections almost exclusively affect hospitalised patients who are SEVERELY immunocompromised — e.g. those who have had part of their immune system removed for a short time while being treated for cancer, or those who have to be artificially immunocompromised after a transplant (solid organ or haematological). Having little or no ability to fight off infection leaves these patients vulnerable to invasive infections, where fungi grow throughout infected organs and sometimes spread via the bloodstream.
These can be extremely difficult to treat, so every effort is made to avoid infection. Air is the main source of infection, both in the operating theatre and in recovery; the main site of infection is the lungs. Indoor air quality is closely monitored in hospitals and (where possible) cleaned via HEPA grade filtration systems. There have also been several research papers that strongly suggest local building works can be a significant factor in hospital outbreaks of invasive aspergillosis. Therefore, local policies have to be put in place to reduce the risk accordingly. Sadly, at the moment such measures do not seem to be completely effective and further work is being carried out to try to detect how spores still manage to infect some patients (there is a possibility that they could be brought in on the clothes of patients and visitors, or found in showers, drinking water and food.
The most common Aspergillus invasive fungal infections are:

Further Reading and Resources on Air Quality
History: John Evelyn’s Fumifugium
John Evelyn (1620-1706) was a 17th century writer, gardener and diarist. Along with his contemporary, Samuel Pepys, he is best known for his diaries. However, Evelyn was a prolific writer, and his publications included works on history, religion, forestry, horticulture, architecture, and law.
Fumifugium, or, The inconveniencie of the aer and smoak of London dissipated together with some remedies humbly proposed by J.E. esq. to His Sacred Majestie, and to the Parliament now assembled was the title that Evelyn gave to his 1661 essay on air pollution in London. Enraged by the heavy smog that often fouled the air in his home city, Evelyn aimed to document the impacts of the smog on people’s health and the environment. He also used the pamphlet (which, as the title suggests, he sent to King Charles II) to put forward a number of solutions that he believed would help to resolve the problem.
Fumifugium is considered to be an early and important example of literature on air quality. Evelyn’s publication demonstrates how discussions and debate around air quality are not just a feature of modern life!
Microbiomes
In 2017, the National Academies of Sciences, Engineering and Medicine (US) produced a comprehensive report exploring microbiomes of the built environment. They provide the following overview:
People’s desire to understand the environments in which they live is a natural one. People spend most of their time in spaces and structures designed, built, and managed by humans, and it is estimated that people in developed countries now spend 90 percent of their lives indoors. As people move from homes to workplaces, traveling in cars and on transit systems, microorganisms are continually with and around them. The human-associated microbes that are shed, along with the human behaviors that affect their transport and removal, make significant contributions to the diversity of the indoor microbiome.
The characteristics of “healthy” indoor environments cannot yet be defined, nor do microbial, clinical, and building researchers yet understand how to modify features of indoor environments—such as building ventilation systems and the chemistry of building materials—in ways that would have predictable impacts on microbial communities to promote health and prevent disease. The factors that affect the environments within buildings, the ways in which building characteristics influence the composition and function of indoor microbial communities, and the ways in which these microbial communities relate to human health and well-being are extraordinarily complex and can be explored only as a dynamic, interconnected ecosystem by engaging the fields of microbial biology and ecology, chemistry, building science, and human physiology.
This report reviews what is known about the intersection of these disciplines, and how new tools may facilitate advances in understanding the ecosystem of built environments, indoor microbiomes, and effects on human health and well-being. It offers a research agenda to generate the information needed so that stakeholders with an interest in understanding the impacts of built environments will be able to make more informed decisions.
Click here to access a full copy of the report.
Indoor (and Healthcare) Air Quality Guidelines
Useful Information for Patients
Workshops and Courses
Institute of Specialist Surveyors and Engineers (UK) run Diploma and Certificate of Education courses in a variety of subjects associated with building. Courses are provided via industry education leader ABBE and require a substantial commitment of up to 500 hours to complete. ISSE graduates have passed the highest standards of training currently available in the UK. If in the UK/EU and are looking for professional training, or if you are a member of the public looking for a surveyor for a damp home, always ensure that the training is to a standard recognised by Ofqual. [N.B. Damp surveyors in the UK commonly refer to a qualification denoted CSRT which used to be the highest qualification routinely attainable in the UK but is, in fact, a 3 day course that is not recognised by Ofqual. Buyer be aware!]
