Date: 26 November 2013
The patient was a 610 g twin male born by spontaneous normal vaginal delivery at 23 weeks and 4 days gestation. He was started on benzyl penicillin and gentamicin for sepsis. On day 3, he developed metabolic acidosis, hyponatremia, anemia, thrombocytopenia and jaundice and his antibiotics were changed to vancomycin, cefotaxime and fluconazole.
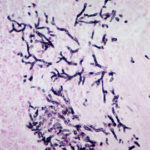
On day 10, multiple circular skin papules with white eschars were noted on his back (Figure A). A full septic screen was repeated including skin scraping and biopsy for urgent microscopy and culture. Microscopy of skin scrapes revealed fungal elements including hyphae and fruiting heads suggestive of Aspergillus spp (Figure B). Lipid amphotericin B was commenced and fluconazole was stopped. Skin scrapings on culture grew Aspergillus fumigatus. A diagnosis of primary cutaneous aspergillosis was made. The patient responded to oral posaconazole 6mg/kg/8 hourly. All lesions disappeared after 44 days and he continued with posaconazole until day 60.
Published case at Langan et al Pediatr Dermatol 2010 Jul-Aug 27 (4) 403-4
Copyright: n/a
Notes:
Images library
-
Title
Legend
-
PtDS2 –Repeated chest infections arrested by itraconazole therapy in ABPA and bronchiectasis
DS2 developed asthma age 24 and now aged 62. From about age 30 she started getting repeated chest infections and a few years later ABPA and bronchiectasis was diagnosed. Infections continued requiring multiple courses of antibiotics annually. At one point DS2 developed a pneumothorax, possibly because of excess coughing. She has chronic rhinitis and mannose binding lectin deficiency. In May 2011, she started itraconazole therapy, and has needed no antibiotic courses for her chest since. Her rhinitis with sinusitis occasionally bothers her. She is delighted to have gone 18 months with no chest infections.
 ,
,  ,
, 
-
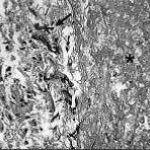
Aspergillus hyphae (arrow) in the lumen without invasion of the necrotic bronchial wall (*) (Nicod 2001).
-
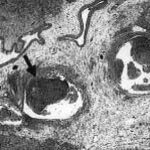
fibrinonecrotic material (arrow) from the airway shown in A, with subocclusion of the bronchial lumen (*)
-
Fibrinous or pseudomembranous bronchitis (arrow) with subocclusion of the airways (* indicates subocclusion of the airways by pseudomembranes)

-
Bronchoscopic biopsy demonstrated septate hyphae with branching at 45o (methenamine silver stain ×400).