Date: 23 January 2014
A 43 year old with smoking related emphysema was admitted to hospital with two separate episodes of haemoptysis. He had been in good health up to 1989, when he was diagnosed as having bilateral pulmonary tuberculosis. At that time a CT scan revealed a cavity in the left upper lobe (20.8cm2) with adjacent confluent infiltrates and pleural thickening. On bronchoscopic examination no abnormalities were noted and endobronchial biopsies did not reveal hyphae.
Over the next 4 years his condition deteriorated and a CT scan showed the left upper lobe cavity had increased to 40cm2. Itraconazole 400mg daily was prescribed. There was some clinical improvement on itraconazole but patient eventually deteriorated with breathlessness and with significant weight loss.
Copyright: n/a
Notes:
Images library
-
Title
Legend
-
PtDS2 –Repeated chest infections arrested by itraconazole therapy in ABPA and bronchiectasis
DS2 developed asthma age 24 and now aged 62. From about age 30 she started getting repeated chest infections and a few years later ABPA and bronchiectasis was diagnosed. Infections continued requiring multiple courses of antibiotics annually. At one point DS2 developed a pneumothorax, possibly because of excess coughing. She has chronic rhinitis and mannose binding lectin deficiency. In May 2011, she started itraconazole therapy, and has needed no antibiotic courses for her chest since. Her rhinitis with sinusitis occasionally bothers her. She is delighted to have gone 18 months with no chest infections.
 ,
,  ,
, 
-
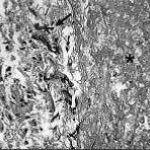
Aspergillus hyphae (arrow) in the lumen without invasion of the necrotic bronchial wall (*) (Nicod 2001).
-
fibrinonecrotic material (arrow) from the airway shown in A, with subocclusion of the bronchial lumen (*)
-
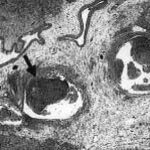
Fibrinous or pseudomembranous bronchitis (arrow) with subocclusion of the airways (* indicates subocclusion of the airways by pseudomembranes)

-
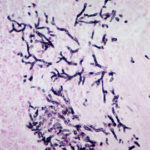
Bronchoscopic biopsy demonstrated septate hyphae with branching at 45o (methenamine silver stain ×400).