Date: 26 November 2013
IPA in late stage AIDS, pt TB
Copyright: n/a
Notes:
Close up of cavity of left upper-lobe, proven to be invasive pulmonary aspergillosis at autopsy.
Pulmonary aspergillosis in a patient who had AIDS for 3 years (CD4 count. <10/mm3). Right middle-lobe consolidation and a left upper-lobe cavity as seen in a previously normal lung; the diagnosis was made by culture of a bronchoalveolar lavage specimen and was confirmed at autopsy. (This was published in (Khoo S, Denning DW. Aspergillus infection in the acquired immune deficiency syndrome. Clin Infect Dis 1994; 19 (suppl 1): S41-48.)
Images library
-
Title
Legend
-
PtDS2 –Repeated chest infections arrested by itraconazole therapy in ABPA and bronchiectasis
DS2 developed asthma age 24 and now aged 62. From about age 30 she started getting repeated chest infections and a few years later ABPA and bronchiectasis was diagnosed. Infections continued requiring multiple courses of antibiotics annually. At one point DS2 developed a pneumothorax, possibly because of excess coughing. She has chronic rhinitis and mannose binding lectin deficiency. In May 2011, she started itraconazole therapy, and has needed no antibiotic courses for her chest since. Her rhinitis with sinusitis occasionally bothers her. She is delighted to have gone 18 months with no chest infections.
 ,
,  ,
, 
-
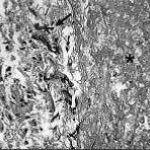
Aspergillus hyphae (arrow) in the lumen without invasion of the necrotic bronchial wall (*) (Nicod 2001).
-
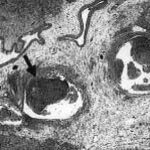
fibrinonecrotic material (arrow) from the airway shown in A, with subocclusion of the bronchial lumen (*)
-
Fibrinous or pseudomembranous bronchitis (arrow) with subocclusion of the airways (* indicates subocclusion of the airways by pseudomembranes)

-
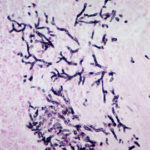
Bronchoscopic biopsy demonstrated septate hyphae with branching at 45o (methenamine silver stain ×400).