Date: 26 November 2013
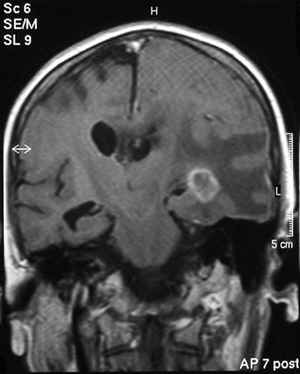
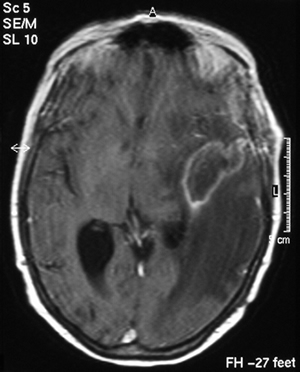
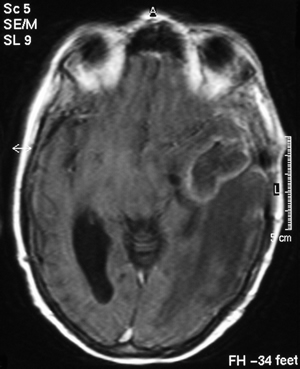
T1 weighted, gadolinium enhanced magnetic resonance brain scan. This 43 year-old alcoholic woman underwent laparoscopic cholecystectomy in January 2001. Ten days after surgery, she became confused, dysphasic and eventually had tonic-clonic seizures. A CT scan showed non-communicating hydrocephalus with ventriculitis. She underwent many complicated neurosurgical interventions, and received long term broad-spectrum antimicrobials and dexamethasone. One month later, she had generalized seizures, and a large abscess was observed on scan (see images). A heavy growth of A. fumigatus was retrieved from the abscess, and amphotericin B and 5-flucytosine were started. Antifungal therapy was changed voriconazole due to intolerance to amphotericin B and worsening disorientation. Voriconazole dosing (which varied from 300mg to 100mg twice daily) was guided by plasma concentrations as enzyme induction with rifampicin and carbamazepine, and reduction in clearance with alcoholic liver disease complicated her voriconazole dosing. Steroids were gradually reduced. She had a good recovery and completed 9 months of voriconazole.
Despite air filtration in the operating rooms, she apparently acquired an intra-operative infection, probably accelerated in presentation by concurrent dexamethasone. Rapid diagnosis and optimization of voriconazole dosing lead to a good outcome.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
PtDS2 –Repeated chest infections arrested by itraconazole therapy in ABPA and bronchiectasis
DS2 developed asthma age 24 and now aged 62. From about age 30 she started getting repeated chest infections and a few years later ABPA and bronchiectasis was diagnosed. Infections continued requiring multiple courses of antibiotics annually. At one point DS2 developed a pneumothorax, possibly because of excess coughing. She has chronic rhinitis and mannose binding lectin deficiency. In May 2011, she started itraconazole therapy, and has needed no antibiotic courses for her chest since. Her rhinitis with sinusitis occasionally bothers her. She is delighted to have gone 18 months with no chest infections.
 ,
,  ,
, 
-
Aspergillus hyphae (arrow) in the lumen without invasion of the necrotic bronchial wall (*) (Nicod 2001).
-
fibrinonecrotic material (arrow) from the airway shown in A, with subocclusion of the bronchial lumen (*)
-
Fibrinous or pseudomembranous bronchitis (arrow) with subocclusion of the airways (* indicates subocclusion of the airways by pseudomembranes)

-
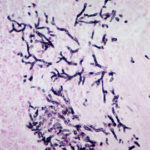
Bronchoscopic biopsy demonstrated septate hyphae with branching at 45o (methenamine silver stain ×400).