Date: 26 November 2013
Patient MD with kyphoscoliosis and chronic cavitary pulmonary aspergillosis and an aspergilloma. Patient exhibited azole resistant A. fumigatus.
Further details
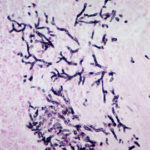
Image A. This CT scan cut shown shows a grossly distorted thorax because of the kyphoscoliosis, a nearly normal appearing left lung, her trachea at an odd angle, demonstrating the normal cartilage rings and an aspergilloma in a cavity which has replaced the right upper lobe. The cavity is surrounded by significant pleural thickening and fibrosis.
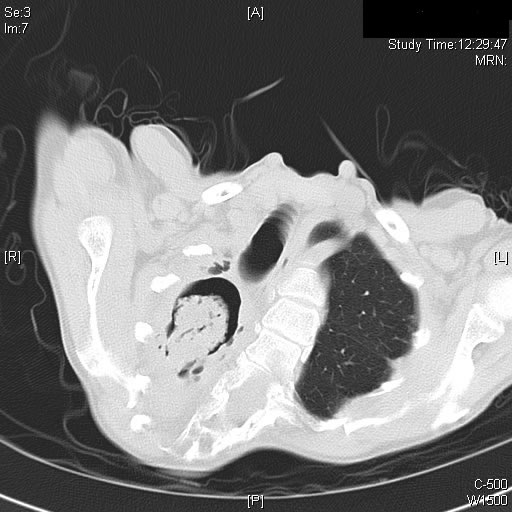
Image B. The other cut (slightly inferior) shows a complex large cavity and some smaller ones posteriorly, with some material consistent with a fungal ball within the large cavity. There is a separate cavity anteriorly and small air spaces within the extensive pleural thickening. Her trachea is widened. the left lung appears normal.
This patient with repaired juvenile scoliosis first recognised that she had pulmonary aspergillosis when she coughed up large amounts of blood, she was admitted to ICU and underwent bronchial artery embolisation, followed by tranexamic acid orally. A. fumigatus was cultured from sputum. A diagnosis of chronic cavitary pulmonary aspergillosis with an aspergilloma was made. She didn’t improve with itraconazole (no fall in Aspergillus precipitins and continuing symptoms, despite good blood levels) and was treated with voriconazole. She had a good sympomatic response, with marginal improvement in her Aspergillus precipitins titre. Remission continued for over 3 years but then her symptoms of cough and general fatigue returned. Her sputum grew A. fumigatus again, which had MICs to itraconazole (>8 mg/L, resistant), voriconazole (8mg/L, resistant) and posaconazole (2mg/mL, resistant). She is being treated with amphotericin B.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
PtDS2 –Repeated chest infections arrested by itraconazole therapy in ABPA and bronchiectasis
DS2 developed asthma age 24 and now aged 62. From about age 30 she started getting repeated chest infections and a few years later ABPA and bronchiectasis was diagnosed. Infections continued requiring multiple courses of antibiotics annually. At one point DS2 developed a pneumothorax, possibly because of excess coughing. She has chronic rhinitis and mannose binding lectin deficiency. In May 2011, she started itraconazole therapy, and has needed no antibiotic courses for her chest since. Her rhinitis with sinusitis occasionally bothers her. She is delighted to have gone 18 months with no chest infections.
 ,
,  ,
, 
-
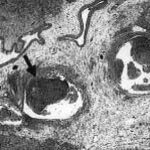
Aspergillus hyphae (arrow) in the lumen without invasion of the necrotic bronchial wall (*) (Nicod 2001).
-
fibrinonecrotic material (arrow) from the airway shown in A, with subocclusion of the bronchial lumen (*)
-
Fibrinous or pseudomembranous bronchitis (arrow) with subocclusion of the airways (* indicates subocclusion of the airways by pseudomembranes)

-
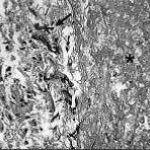
Bronchoscopic biopsy demonstrated septate hyphae with branching at 45o (methenamine silver stain ×400).