Date: 26 November 2013
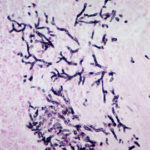
Aspergillus terreus Thom. Conidial head of Aspergillus terreus. Conidial heads are compact, columnar and biseriate. Conidiophores are hyaline to slightly yellow and smooth walled.
Copyright:
With thanks to G Kaminski. D Ellis and R Hermanis Mycology Unit, Women’s & Children’s Hospital , Adelaide, South Australia 5006
Notes:
Colonies on CYA 40-50 mm diam, plane, low and velutinous, usually quite dense; mycelium white; conidial production heavy, brown (Dark Blonde to Camel, 5-6D4); reverse pale to dull brown or yellow brown. Colonies on MEA 40-60 mm diam, similar to those on CYA or less dense. Colonies on G25N 18-22 mm diam, plane or irregularly wrinkled, low and sparse; conidial production light, pale brown; brown soluble pigment sometimes produced; reverse brown. No growth at 5°C. Colonies at 37°C growing very rapidly, 50 mm or more diam, of similar appearance to those on CYA at 25°C.Conidiophores borne from surface hyphae, stipes 100-250 μm long, smooth walled; vesicles 15-20 μm diam, fertile over the upper hemisphere, with densely packed, short, narrow metulae and phialides, both 5-8 μm long; conidia spherical, very small, 1.8-2.5 μm diam, smooth walled, at maturity borne in long, well defined columns.Distinctive featuresVelutinous colonies formed at both 25°C and 37°C, uniformly brown, with no other colouration, and minute conidia borne in long columns make Aspergillus terreus a distinctive species.
Images library
-
Title
Legend
-
PtDS2 –Repeated chest infections arrested by itraconazole therapy in ABPA and bronchiectasis
DS2 developed asthma age 24 and now aged 62. From about age 30 she started getting repeated chest infections and a few years later ABPA and bronchiectasis was diagnosed. Infections continued requiring multiple courses of antibiotics annually. At one point DS2 developed a pneumothorax, possibly because of excess coughing. She has chronic rhinitis and mannose binding lectin deficiency. In May 2011, she started itraconazole therapy, and has needed no antibiotic courses for her chest since. Her rhinitis with sinusitis occasionally bothers her. She is delighted to have gone 18 months with no chest infections.
 ,
,  ,
, 
-
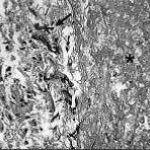
Aspergillus hyphae (arrow) in the lumen without invasion of the necrotic bronchial wall (*) (Nicod 2001).
-
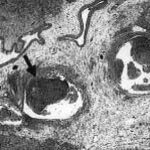
fibrinonecrotic material (arrow) from the airway shown in A, with subocclusion of the bronchial lumen (*)
-
Fibrinous or pseudomembranous bronchitis (arrow) with subocclusion of the airways (* indicates subocclusion of the airways by pseudomembranes)

-
Bronchoscopic biopsy demonstrated septate hyphae with branching at 45o (methenamine silver stain ×400).