Date: 26 November 2013
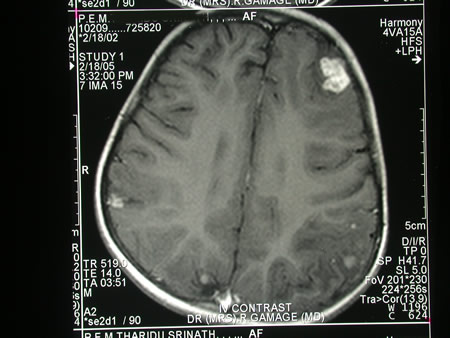
Image c. 3 yr old boy with CNS aspergillosis pt TS. MRI scan pre-amphotericin B
Copyright: n/a
Notes:
A 3 year old boy, quite active and healthy clinically, who has CNS aspergillosis. He was first seen about 4 months ago for a red eye, which turned out to be panophthalmitis; culture yielded Aspergillus spp. He received 2 weeks of iv amphotericin and was sent home by the ophthalmologists. No h/o eye trauma. He returned 2 weeks ago with focal fits, and the MR showed several lesions bilaterally (including ring enhancing lesions) and normal sinuses, and a brain bx showed fungal hyphae (no culture this time). His immune status (normal WCC and neutrophil function so far) was investigated.
He was given conventional amphotericin for 8 weeks, and switched to oral itraconazole. We had to limit the ampho to 0.7 mg/kg owing to toxicity (mainly hypokalaemia).
The MRI scan was repeated at about 6 weeks, and generally showed good improvement (scans e-h). The enhancement/flare were gone but remained in a few lesions, the lesions themselves were all either gone or much smaller. Further investigations revealed the child was immunocompetent.
Patient was switched from amphotericin to oral itraconazole at week 8 essentially on a clinical assessment. Awaiting follow-up.
Images library
-
Title
Legend
-
PtDS2 –Repeated chest infections arrested by itraconazole therapy in ABPA and bronchiectasis
DS2 developed asthma age 24 and now aged 62. From about age 30 she started getting repeated chest infections and a few years later ABPA and bronchiectasis was diagnosed. Infections continued requiring multiple courses of antibiotics annually. At one point DS2 developed a pneumothorax, possibly because of excess coughing. She has chronic rhinitis and mannose binding lectin deficiency. In May 2011, she started itraconazole therapy, and has needed no antibiotic courses for her chest since. Her rhinitis with sinusitis occasionally bothers her. She is delighted to have gone 18 months with no chest infections.
 ,
,  ,
, 
-
Aspergillus hyphae (arrow) in the lumen without invasion of the necrotic bronchial wall (*) (Nicod 2001).
-
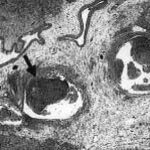
fibrinonecrotic material (arrow) from the airway shown in A, with subocclusion of the bronchial lumen (*)
-
Fibrinous or pseudomembranous bronchitis (arrow) with subocclusion of the airways (* indicates subocclusion of the airways by pseudomembranes)

-
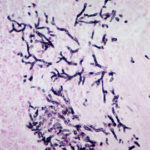
Bronchoscopic biopsy demonstrated septate hyphae with branching at 45o (methenamine silver stain ×400).