Date: 26 November 2013
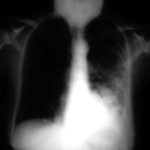
Image A. This 25 year old woman was previously well and presented with a pneumonia of uncertain aetiology. She has infiltrates in right upper-lobe and left middle and lower zones. The diagnosis was later made of chronic invasive pulmonary aspergillosis by bronchoscopy . Subsequently she was diagnosed with adult-onset chronic granulomatous disease with neutrophil function assays.
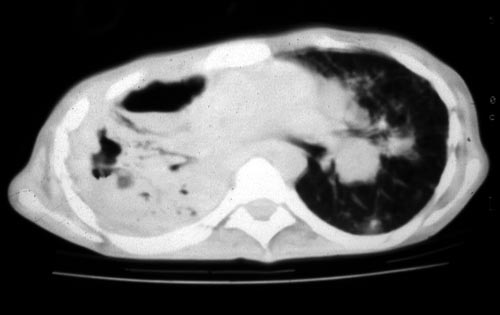
Image B. CT scan of the thorax just below the carina, showing almost complete opacification of the right lung and marked nodular shadowing around the hilum of the left lung.
Image C. Progression of pulmonary infiltrates are seen seven weeks later, despite administration of amphotericin B.
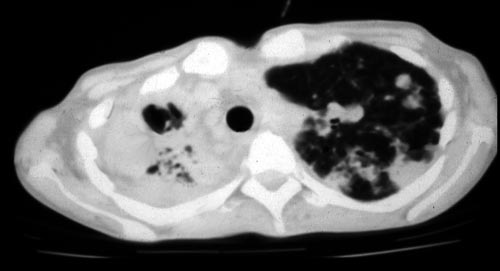
Image D. CT scan of the thorax above the carina showing near complete opacification of the right lung and multiple discrete nodular shadows in the left lung.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
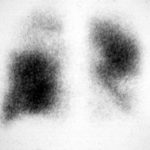
25/04/90 After itraconazole treatment. Major improvement, defined as a complete response, after 10 weeks therapy with itraconazole.

-
Image A. Chest x-ray shows a single nodule in the left mid lung field.
Image B. This emphasises how chest x-rays in this context underestimate the extent of disease. The most anterior nodule has ground glass surrrounding the nodule, a halo sign. This diagnostic feature is missed on plain chest X-rays.
 ,
, 
-
Chest X ray after 4 days, prior to treatment, showing massive increase in volume of lesion (Fig 2)

-
Image A. This patient, aged 25 years developed a non productive cough and dyspnoea in the context of late-stage AIDS, CMV disease with ganciclovir-induced neutropenia and receiving corticosteroids. His chest radiograph shows fine bilateral reticular lower-lobe shadowing. He then developed gastro-intestinal bleeding with a gastric ulcer which showed hyphae on biopsy. He then developed blindness of one eye and the globe of his eye perforated. Hyphae were seen and Aspergillus cultured from the vitreous aspirate.
Image B. This radiograph, taken 25 days after the first and 3 days before death, shows of fine bilateral lower-lobe reticular shadows progressing to nodules in all lung zones.
This patient was reported as patient 3 in Denning DW, Follansbee S, Scolaro M, Norris S, Edelstein D, Stevens DA. Pulmonary aspergillosis in the acquired immunodeficiency syndrome. N Engl J Med 1991; 324: 654-662.
 ,
, 
-
Further details
Image A. Bronchoscopy revealed Aspergillus on culture.
Image B. The ability of Aspergillus to cause pulmonary infarction, probably through direct angioinvasion in this case, is characteristic.
 ,
, 
-
(Fig 1) Chest radiograph with ‘classical’ appearance of a pulmonary infarction – a wedge-shaped lesion peripherally set against the pleura.

-
Large soft left upper-lobe shadow of focal invasive pulmonary aspergillosis in leukaemia, that was missed on earlier radiographs but apparent retrospectively. Variable density of the lesion suggests cavitation, which would be clearly visible on a CT scan of the thorax.

-
Severe unilateral invasive aspergillosis of the left lung, with complete consolidation of the left lower-lobe and reticular shadowing extending up into the left upper lobe. The right lung appears normal.