Date: 26 November 2013
A Bronchogram showing saccular bronchiectasis
Copyright:
Fungal Infection Trust
Notes:
Bronchography (A & B)is an old technique for visualising the bronchial tree, by introducing radio-opaque dye into the airways and then taking a chest Xray. It was the first means used to diagnose bronchiectasis, seen in these examples below. An historical description of the technique from 1922 can be seen here
Nowadays CT scanning of the chest is used for this purpose with 3D reconstruction in some cases.
White cell scan (C) This pair of white cell scans from different people show almost no white cells in the lungs on the left, as in a healthy person (the spleen is the ‘hottest area). The scan on the right shows grossly increased update, especially in the left lung (seen on the right). This is the typical feature of severe bronchiectasis with large amounts of neutrophils and other phagocytes present.
Sinusitis Plain X-ray (D) of the face showing the maxillary sinuses. The right maxillary sinus is complete fluid filled and the left side (seen on the right) has a fluid level. These features may be seen with severe acute bacterial sinusitis, but also other causes of sinusitis, including allergic rhinosinusitis.
Images library
-
Title
Legend
-
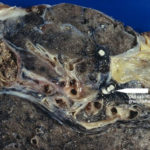
Macroscopic view medial aspect of left upper lobe of lung showing segmental collapse and congestion of lower segments, with mucus extruding from incised bronchi.
 ,
,  ,
,  ,
,  ,
, 
-
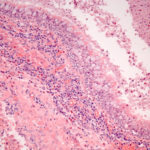
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.