Date: 26 November 2013
Copyright: n/a
Notes:
Dr. Balajee is a graduate of the University of Madras (India) and completed her post doctoral training in Dr. Kieren Marr’s laboratory at the Fred Hutchinson Cancer Research Center, Seattle, US. Currently she leads the Molecular Epidemiology Unit within the Mycotic Diseases Branch at the Centers for Disease Control and Prevention.
Dr. Balajee’s dynamic research program is focused on public health mycology that includes studies on the molecular epidemiology of medically important fungi, specifically the genus Aspergillus. Another area of interest is understanding the role of mycotoxins, specifically aflatoxin elaborated by Aspergillus in mediating adverse health effects in humans. Dr. Balajee has published over 25 peer-reviewed articles and several book chapters and is committed to creating a learning environment for budding public health mycologists in her laboratory. Dr. Balajee is the convenor for an international working group on A. terreus to gather and disseminate scientific knowledge in this field and is a member of the working group on species concepts inAspergillus.
Key Contributions to recent literature:
- Balajee SA, Weaver M, Imhof A, Gribskov J, Marr KA. Aspergillus fumigatus variant with decreased susceptibility to multiple antifungals. Antimicrob Agents Chemother. 2004 Apr;48(4):1197-203.
- Balajee SA, Imhof A, Gribskov JL, Marr KA. Determination of antifungal drug susceptibilities of Aspergillus species by a fluorescence-based microplate assay. J Antimicrob Chemother. 2005 Jan;55(1):102-5.
- Balajee SA, Gribskov JL, Hanley E, Nickle D, Marr KA. Aspergillus lentulus sp. nov., a new sibling species of A. fumigatus.Eukaryot Cell. 2005 Mar; 4(3):625-32.
- Bok JW, Chung D, Balajee SA, Marr KA, Andes D, Nielsen KF, Frisvad JC, Kirby KA, Keller NP. GliZ, a transcriptional regulator of gliotoxin biosynthesis, contributes to Aspergillus fumigatusvirulence. Infect Immun. 2006 Dec; 74(12):6761-8.
- Balajee SA, Nickle D, Varga J, Marr KA. Molecular studies reveal frequent misidentification of Aspergillus fumigatus by morphotyping. 2006 Oct; 5(10):1705-12.Eukaryot Cell.
- Balajee SA, Lindsley MD, Iqbal N, Ito J, Pappas PG, Brandt ME. A non-sporulating clinical isolate identified as Petromyces alliaceus (anamorph Aspergillus alliaceus) by morphological and sequence based methods. J Clin Microbiol. 2007 Aug; 45(8):2701-3.
- Balajee SA, Tay ST, A Lasker B, Hurst SF, Rooney AP.Characterization of a novel gene for strain typing reveals substructuring of Aspergillus fumigatus across North America.Eukaryot Cell. 2007 Aug; 6 (8):1392-9.
- Balajee SA, L Sigler and ME Brandt. DNA and the classical way: identification of medically important molds in the 21st century.Med Mycol 2007; 45: 1-16
- Balajee SA, SS Magill, ME Brandt. The role of molecular methods in the identification of fungal infections. Curr Fung Infect Reports 2007; 1: in press.
- Kano R, K Itamoto, M Okuda, H Inokuma, A Hasegawa, SA Balajee. Isolation of Aspergillus udagawae from a fatal case of feline orbital aspergillosis. Mycoses 2008 (in press).
- Balajee S.A, J. Houbraken, P.E. Verweij, S-B. Hong, T. Yaghuchi, J. Varga and R.A. Samson2. Aspergillus species identification in the clinical setting. Studies in Mycology. 59: 39–46. 2007.
- Balajee SA, de Valk HA, Lasker BA, Meis JF, Klaassen CH. J Microbiol Methods. 2008 Feb 23. Epub. Utility of a microsatellite assay for identifying clonally related outbreak isolates ofAspergillus fumigatus.
Arun Balajee Ph.D.
Chief, Molecular Epidemiology Unit,
Mycotic Diseases Branch,
Centers for Disease Control and Prevention Mail stop – G 11 1600 Clifton Road, Atlanta, GA – 30333
Email fir3@cdc.gov
Phone – 404 639 3337
Fax – 404 639 3546
Images library
-
Title
Legend
-
Image A. Scan shows large bore needle in one of the cavities on the right. The contrast media is mixed with amphotericin B and is whiter than surrounding lung tissue and fungal ball. The contrast surrounds the aspergilloma present in this cavity. Some of the contrast has fallen by gravity in another cavity anteriorly below the one being injected, showing communication between the cavities.
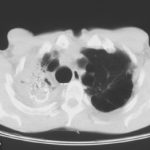
Image B. Scan showing contrast media mixed with amphotericin B injected into a multicystic cavity in the right upper lobe. The contrast (white) flows around the aspergilloma present in this cavity. The contrast falls by gravity posteriorly.
Image C. The opposite lung shows multiple empty cystic spaces with little normal lung.
Image D. There is substantial pleural thickening surrounding the irregular cavity containing the aspergilloma.
 ,
,  ,
,  ,
, 
-
Extensive multilobar, varicose bronchiectasis, with some cyst formation most marked on the left anteriorly. Also some inhomogeneity of the pulmonary parenchyma secondary to air trapping in several affected segments.
-
CT scans of thorax. Anterior left-sided bronchiectasis with extensive mucous plugging and with some proximal bronchiectasis and plugging on the right.

-
Bilateral multilobar varicose bronchiectasis affecting the segmental and small order bronchi, with some distal plugging.
-
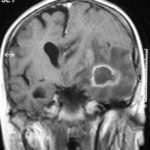
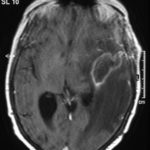
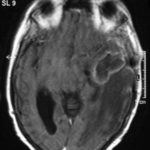
T1 weighted, gadolinium enhanced magnetic resonance brain scan. This 43 year-old alcoholic woman underwent laparoscopic cholecystectomy in January 2001. Ten days after surgery, she became confused, dysphasic and eventually had tonic-clonic seizures. A CT scan showed non-communicating hydrocephalus with ventriculitis. She underwent many complicated neurosurgical interventions, and received long term broad-spectrum antimicrobials and dexamethasone. One month later, she had generalized seizures, and a large abscess was observed on scan (see images). A heavy growth of A. fumigatus was retrieved from the abscess, and amphotericin B and 5-flucytosine were started. Antifungal therapy was changed voriconazole due to intolerance to amphotericin B and worsening disorientation. Voriconazole dosing (which varied from 300mg to 100mg twice daily) was guided by plasma concentrations as enzyme induction with rifampicin and carbamazepine, and reduction in clearance with alcoholic liver disease complicated her voriconazole dosing. Steroids were gradually reduced. She had a good recovery and completed 9 months of voriconazole.
Despite air filtration in the operating rooms, she apparently acquired an intra-operative infection, probably accelerated in presentation by concurrent dexamethasone. Rapid diagnosis and optimization of voriconazole dosing lead to a good outcome.
 ,
,  ,
,  ,
,  ,
,  ,
, 
-
Allergic Broncho-pulmonary aspergillosis. Pt CT. Extensive severe saccular bronchiectasis of the left lower lobe and to a lesser extent of the left upper and right lower lobe.
-
Ct scan of chest. This patient with severe ABPA, serologically and radiologically, developed a spectrum of lesions in the lung. In this cut, a cavitating infiltrate in the anterior segment of the left upper lobe was visualised together with some bronchial thickening and bronchiectasis in the left upper and lower lobe.



 ,
,  ,
,  ,
,