Date: 26 November 2013
Copyright: n/a
Notes:
Dr. Balajee is a graduate of the University of Madras (India) and completed her post doctoral training in Dr. Kieren Marr’s laboratory at the Fred Hutchinson Cancer Research Center, Seattle, US. Currently she leads the Molecular Epidemiology Unit within the Mycotic Diseases Branch at the Centers for Disease Control and Prevention.
Dr. Balajee’s dynamic research program is focused on public health mycology that includes studies on the molecular epidemiology of medically important fungi, specifically the genus Aspergillus. Another area of interest is understanding the role of mycotoxins, specifically aflatoxin elaborated by Aspergillus in mediating adverse health effects in humans. Dr. Balajee has published over 25 peer-reviewed articles and several book chapters and is committed to creating a learning environment for budding public health mycologists in her laboratory. Dr. Balajee is the convenor for an international working group on A. terreus to gather and disseminate scientific knowledge in this field and is a member of the working group on species concepts inAspergillus.
Key Contributions to recent literature:
- Balajee SA, Weaver M, Imhof A, Gribskov J, Marr KA. Aspergillus fumigatus variant with decreased susceptibility to multiple antifungals. Antimicrob Agents Chemother. 2004 Apr;48(4):1197-203.
- Balajee SA, Imhof A, Gribskov JL, Marr KA. Determination of antifungal drug susceptibilities of Aspergillus species by a fluorescence-based microplate assay. J Antimicrob Chemother. 2005 Jan;55(1):102-5.
- Balajee SA, Gribskov JL, Hanley E, Nickle D, Marr KA. Aspergillus lentulus sp. nov., a new sibling species of A. fumigatus.Eukaryot Cell. 2005 Mar; 4(3):625-32.
- Bok JW, Chung D, Balajee SA, Marr KA, Andes D, Nielsen KF, Frisvad JC, Kirby KA, Keller NP. GliZ, a transcriptional regulator of gliotoxin biosynthesis, contributes to Aspergillus fumigatusvirulence. Infect Immun. 2006 Dec; 74(12):6761-8.
- Balajee SA, Nickle D, Varga J, Marr KA. Molecular studies reveal frequent misidentification of Aspergillus fumigatus by morphotyping. 2006 Oct; 5(10):1705-12.Eukaryot Cell.
- Balajee SA, Lindsley MD, Iqbal N, Ito J, Pappas PG, Brandt ME. A non-sporulating clinical isolate identified as Petromyces alliaceus (anamorph Aspergillus alliaceus) by morphological and sequence based methods. J Clin Microbiol. 2007 Aug; 45(8):2701-3.
- Balajee SA, Tay ST, A Lasker B, Hurst SF, Rooney AP.Characterization of a novel gene for strain typing reveals substructuring of Aspergillus fumigatus across North America.Eukaryot Cell. 2007 Aug; 6 (8):1392-9.
- Balajee SA, L Sigler and ME Brandt. DNA and the classical way: identification of medically important molds in the 21st century.Med Mycol 2007; 45: 1-16
- Balajee SA, SS Magill, ME Brandt. The role of molecular methods in the identification of fungal infections. Curr Fung Infect Reports 2007; 1: in press.
- Kano R, K Itamoto, M Okuda, H Inokuma, A Hasegawa, SA Balajee. Isolation of Aspergillus udagawae from a fatal case of feline orbital aspergillosis. Mycoses 2008 (in press).
- Balajee S.A, J. Houbraken, P.E. Verweij, S-B. Hong, T. Yaghuchi, J. Varga and R.A. Samson2. Aspergillus species identification in the clinical setting. Studies in Mycology. 59: 39–46. 2007.
- Balajee SA, de Valk HA, Lasker BA, Meis JF, Klaassen CH. J Microbiol Methods. 2008 Feb 23. Epub. Utility of a microsatellite assay for identifying clonally related outbreak isolates ofAspergillus fumigatus.
Arun Balajee Ph.D.
Chief, Molecular Epidemiology Unit,
Mycotic Diseases Branch,
Centers for Disease Control and Prevention Mail stop – G 11 1600 Clifton Road, Atlanta, GA – 30333
Email fir3@cdc.gov
Phone – 404 639 3337
Fax – 404 639 3546
Images library
-
Title
Legend
-
Pt AR Interval development of chronic cavitary pulmonary aspergillosis in the context of sarcoidosis
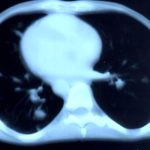
This patient was diagnosed with sarcoid after developing a chronic cough with the attached chest X-ray. In February 2003 the X-ray demonstrated bilateral extensive changes consistent with fibrocystic sarcoidosis with a complex cavitary area in both apices, more marked on the right. She was given a course of corticosteroids.

-
Further details
Image B. Additional cavities are apparent inferior to this large cavity and are in communication both with the bronchi and the additional cavities. Some of the apparent cavities are probably dilated bronchi. The left lower lung is completely opacified otherwise. The degree of pleural fibrosis surrounding the left apical cavity is reduced slightly over the interval of four months.
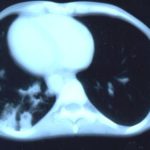
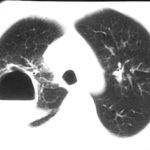
Image C. This shows an almost normal hyperexpanded right lung with a very substantially contracted left lung with one large airway visible and probably incontinuity with a slightly irregular cavity containing some debris, presumably fungal tissue. Other levels show very large left apical cavity with numerous subsections containing debris or fibrotic tissue and almost complete fibrosis of the lung below the level of the carina on the left, with some calcification within the fibrotic lung tissue.
 ,
,  ,
, 
-
Transverse sections through the thorax of a patient with AIDS, hepatitis C and a left tempero-parietal cerebral lymphoma. His CD4 cell count was 45 x 106 / l. The lymphoma was proven by biopsy after a poor response to anti-toxoplasma therapy. He was given dexamethasone to cover the surgery and then developed diabetes mellitus. He did not receive chemotherapy for his lymphoma but did have 2 cerebral radiotherapy treatments (1.8 Gy each). Three weeks after the biopsy he developed dyspnoea and fever. Shortly after this he developed a right-sided hemiparesis, became comatose and died 2 days later.Autopsy showed a cerebral lymphoma and pulmonary and renal aspergillosis. Aspergillus nidulans was recovered from cultures of lungs and kidney.
 ,
,  ,
,  ,
, 
-
Fever chart of Pt CA -heart transplant pt with candidemia on amphotericin therapy, who developed pulmonary aspergillosis.

-
A Colonies on MEA + 20% sucrose after two weeks; B ascomata, x 40; C conidia and conidiophore, x 920; D ascospores and conidia x2330; E portion of ascoma with asci x920

-
A 66 yr old patient in good general health developed onychomycosis. Samples taken from the affected nail were grown by culture and examined by microscopy. Oral itraconazole pulse therapy was given to the patient (200 mg twice daily for 1 week, with 3 weeks off between successive pulses, for four pulses) and treatment was successful.




 ,
,  ,
,  ,
,  ,
,  ,
, 
 ,
,  ,
, 