Date: 26 November 2013
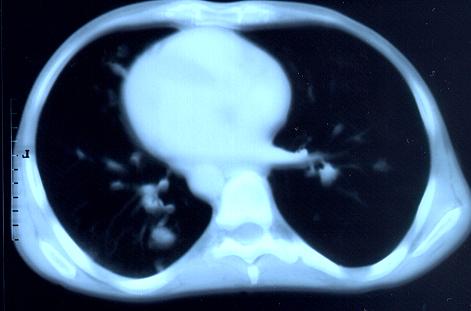
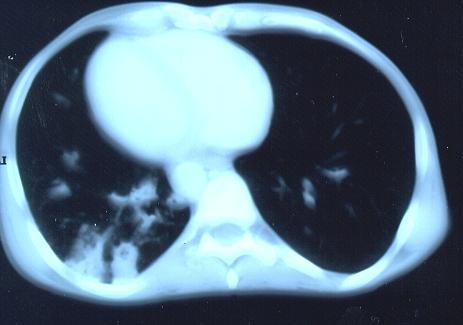
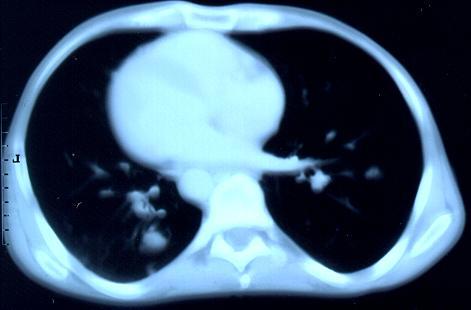
Transverse sections through the thorax of a patient with AIDS, hepatitis C and a left tempero-parietal cerebral lymphoma. His CD4 cell count was 45 x 106 / l. The lymphoma was proven by biopsy after a poor response to anti-toxoplasma therapy. He was given dexamethasone to cover the surgery and then developed diabetes mellitus. He did not receive chemotherapy for his lymphoma but did have 2 cerebral radiotherapy treatments (1.8 Gy each). Three weeks after the biopsy he developed dyspnoea and fever. Shortly after this he developed a right-sided hemiparesis, became comatose and died 2 days later.Autopsy showed a cerebral lymphoma and pulmonary and renal aspergillosis. Aspergillus nidulans was recovered from cultures of lungs and kidney.
Copyright:
Images submitted by Dr. Cornelia Lass-Floerl, University of Innsbruck – Institute of Hygiene; the case team includes: Dr. Mario Sarcletti, Dr. Alfons Stöger and Prof. Hans Maier all at the University of Innsbruck.
Notes: n/a
Images library
-
Title
Legend
-
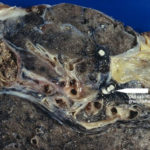
Macroscopic view medial aspect of left upper lobe of lung showing segmental collapse and congestion of lower segments, with mucus extruding from incised bronchi.
 ,
,  ,
,  ,
,  ,
, 
-
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.