Date: 26 November 2013
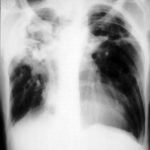
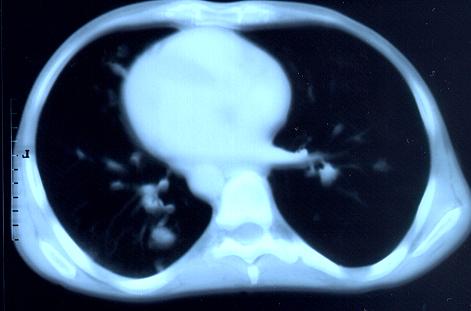
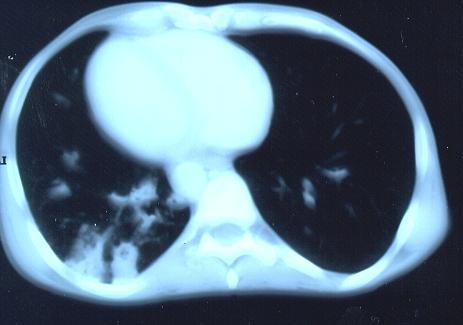
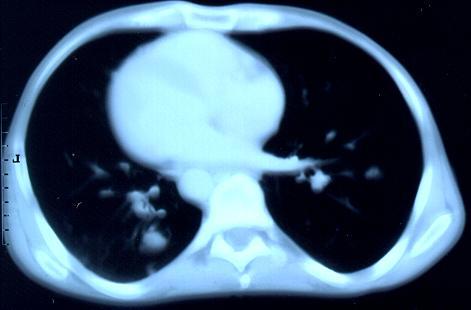
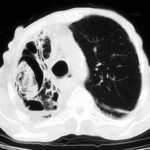
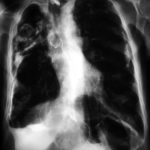
Transverse sections through the thorax of a patient with AIDS, hepatitis C and a left tempero-parietal cerebral lymphoma. His CD4 cell count was 45 x 106 / l. The lymphoma was proven by biopsy after a poor response to anti-toxoplasma therapy. He was given dexamethasone to cover the surgery and then developed diabetes mellitus. He did not receive chemotherapy for his lymphoma but did have 2 cerebral radiotherapy treatments (1.8 Gy each). Three weeks after the biopsy he developed dyspnoea and fever. Shortly after this he developed a right-sided hemiparesis, became comatose and died 2 days later.Autopsy showed a cerebral lymphoma and pulmonary and renal aspergillosis. Aspergillus nidulans was recovered from cultures of lungs and kidney.
Copyright:
Images submitted by Dr. Cornelia Lass-Floerl, University of Innsbruck – Institute of Hygiene; the case team includes: Dr. Mario Sarcletti, Dr. Alfons Stöger and Prof. Hans Maier all at the University of Innsbruck.
Notes: n/a
Images library
-
Title
Legend
-
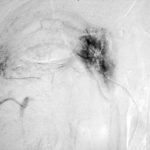
Late (venous) phase angiogram of a right intercostal artery showing persistence of vascular blush and further filling of a branch of the pulmonary artery.
-
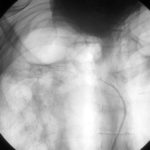
Catheter tip in a right posterior intercostal artery on screening film.
-
Angiogram of a right bronchial artery on subtraction film in the early arterial phase showing filling hypervascular circulation superiorly and communications with a pulmonary arterial radical.

-
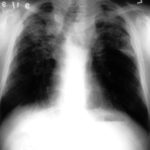
This patient with severe pulmonary sarcoidosis has bilateral aspergillomas. A rim of air is visible around parts of the aspergillomas on both sides. This patient was recruited into the NIAID Mycoses Study Group multicentre study of the treatment of invasive pulmonary aspergillosis with itraconazole but not analysed because invasive disease was not demonstrated. Denning DW, Lee JY, Hostetler JS, Pappas P, Kauffman CA, Dewsnup DH, Galgiani JN, Graybill JR, Sugar AM, Catanzaro A, Gallis H, Perfect JR, Dockery B, Dismukes WE, Stevens DA, NIAID Mycoses Study Group multicenter trial of oral itraconazole therapy of invasive aspergillosis. Am J Med 1994; 97: 135-144
-
Extensive pleural thickening is demonstrated at the left apex on this CT scan of a woman who had previously had tuberculosis and whose large cavity gradually became obliterated by pleural thickening. An aspergilloma is demonstrable within the cavity

-
This chest radiograph (AMBER film) demonstrates the typical extensive pleural thickening at the right apex, seen in patients with aspergillomas. The cavity appears not to contain an aspergilloma but on CT scan had some ‘debris’ and Aspergillus antibiotics (precipitins) were strongly positive. The differential diagnosis lies between an aspergilloma and chronic invasive pulmonary aspergillosis. The extensive pleural thickening is heavily in favour of an aspergilloma, even without a well demonstrated fungal ball in the cavity.

-
Image C. Another example of a severe apical aspergilloma with remarkably little pleural thickening on plain chest radiograph (AMBER film). Severe distortion of the trachea is demonstrated.
 ,
,  ,
, 
-
Right apical aspergilloma, patient WC. Plain chest radiograph of patient with right apical aspergilloma in an old, large tuberculous cavity. Severe haemoptysis and respiratory insufficiency together constituted the indications for embolisation which was done in one session over a 3 hour period (see images 1-6).