Date: 21 January 2014
Further details
Image B. Additional cavities are apparent inferior to this large cavity and are in communication both with the bronchi and the additional cavities. Some of the apparent cavities are probably dilated bronchi. The left lower lung is completely opacified otherwise. The degree of pleural fibrosis surrounding the left apical cavity is reduced slightly over the interval of four months.
Image C. This shows an almost normal hyperexpanded right lung with a very substantially contracted left lung with one large airway visible and probably incontinuity with a slightly irregular cavity containing some debris, presumably fungal tissue. Other levels show very large left apical cavity with numerous subsections containing debris or fibrotic tissue and almost complete fibrosis of the lung below the level of the carina on the left, with some calcification within the fibrotic lung tissue.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
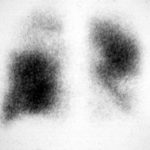
25/04/90 After itraconazole treatment. Major improvement, defined as a complete response, after 10 weeks therapy with itraconazole.

-
Image A. Chest x-ray shows a single nodule in the left mid lung field.
Image B. This emphasises how chest x-rays in this context underestimate the extent of disease. The most anterior nodule has ground glass surrrounding the nodule, a halo sign. This diagnostic feature is missed on plain chest X-rays.
 ,
, 
-
Chest X ray after 4 days, prior to treatment, showing massive increase in volume of lesion (Fig 2)

-
Image A. This patient, aged 25 years developed a non productive cough and dyspnoea in the context of late-stage AIDS, CMV disease with ganciclovir-induced neutropenia and receiving corticosteroids. His chest radiograph shows fine bilateral reticular lower-lobe shadowing. He then developed gastro-intestinal bleeding with a gastric ulcer which showed hyphae on biopsy. He then developed blindness of one eye and the globe of his eye perforated. Hyphae were seen and Aspergillus cultured from the vitreous aspirate.
Image B. This radiograph, taken 25 days after the first and 3 days before death, shows of fine bilateral lower-lobe reticular shadows progressing to nodules in all lung zones.
This patient was reported as patient 3 in Denning DW, Follansbee S, Scolaro M, Norris S, Edelstein D, Stevens DA. Pulmonary aspergillosis in the acquired immunodeficiency syndrome. N Engl J Med 1991; 324: 654-662.
 ,
, 
-
Further details
Image A. Bronchoscopy revealed Aspergillus on culture.
Image B. The ability of Aspergillus to cause pulmonary infarction, probably through direct angioinvasion in this case, is characteristic.
 ,
, 
-
(Fig 1) Chest radiograph with ‘classical’ appearance of a pulmonary infarction – a wedge-shaped lesion peripherally set against the pleura.

-
Large soft left upper-lobe shadow of focal invasive pulmonary aspergillosis in leukaemia, that was missed on earlier radiographs but apparent retrospectively. Variable density of the lesion suggests cavitation, which would be clearly visible on a CT scan of the thorax.

-
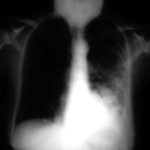
Severe unilateral invasive aspergillosis of the left lung, with complete consolidation of the left lower-lobe and reticular shadowing extending up into the left upper lobe. The right lung appears normal.