Date: 26 November 2013
The patient was a 610 g twin male born by spontaneous normal vaginal delivery at 23 weeks and 4 days gestation. He was started on benzyl penicillin and gentamicin for sepsis. On day 3, he developed metabolic acidosis, hyponatremia, anemia, thrombocytopenia and jaundice and his antibiotics were changed to vancomycin, cefotaxime and fluconazole.
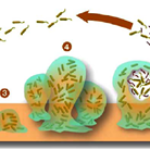
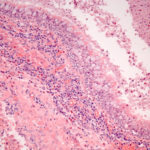
On day 10, multiple circular skin papules with white eschars were noted on his back (Figure A). A full septic screen was repeated including skin scraping and biopsy for urgent microscopy and culture. Microscopy of skin scrapes revealed fungal elements including hyphae and fruiting heads suggestive of Aspergillus spp (Figure B). Lipid amphotericin B was commenced and fluconazole was stopped. Skin scrapings on culture grew Aspergillus fumigatus. A diagnosis of primary cutaneous aspergillosis was made. The patient responded to oral posaconazole 6mg/kg/8 hourly. All lesions disappeared after 44 days and he continued with posaconazole until day 60.
Published case at Langan et al Pediatr Dermatol 2010 Jul-Aug 27 (4) 403-4
Copyright: n/a
Notes:
Images library
-
Title
Legend
-
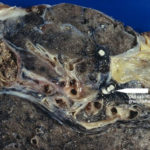
Macroscopic view medial aspect of left upper lobe of lung showing segmental collapse and congestion of lower segments, with mucus extruding from incised bronchi.
 ,
,  ,
,  ,
,  ,
, 
-
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.