Date: 26 November 2013
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.
Copyright:
Fungal Research Trust
Notes: n/a
Images library
-
Title
Legend
-
A Colonies on MEA after one week, B conidial head x920, C atypical reduced conidial head x920, D conidial head x 920.

-
A case of onychomycosis associated with Aspergillus ochraceopetaliformis as described in Med Mycol. 2009 Mar 9:1-5, 2009,Brasch J, Varga J, Jensen JM, Egberts F & Tintelnot K

-
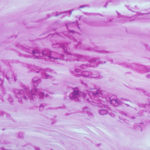
Histology of the infected nail (PAS stain) showing thick fungal elements and septate hyphae within nail material.
-
culture and identified in a case of onychomycosis – Culture at higher magnification.
-
culture and identified in a case of onychomycosis – Culture of Aspergillus ochraceopetaliformis on Sabouraud agar with cycloheximide at 26C

-
This patient with chronic cavitary pulmonary aspergillosis was treated with itraconazole, with some success, but considerable gastrointestinal disturbance (diarrhoea, flatulence and uncomfortable feeling in his abdomen). He also developed a facial rash. Itraconazole was stopped and he reverted to voriconazole which he was unable to take because of a severe feeling of being generally unwell. His facial rash resolved. Application was made for funding posaconazole. He started this and after 6 weeks an almost identical facial rash to that seen with itraconazole appeared. He tolerated posaconazole well in other respects, and his chronic cavitary pulmonary aspergillosis is now significantly better (symptomatically and serologically). July 2007
 ,
,  ,
,  ,
, 
-
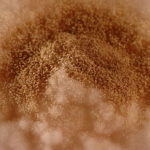
This patient with ABPA and chronic cavitary pulmonary aspergillosis has been stabilized on voriconazole treatment for >5 years. She had a degree of photosensitivity most of that time, noticed early in the course of voriconazole treatment. She is oxygen and wheelchair dependent and doesn’t go outside very much, so most of her light exposure has been indoor light. She developed rough scaly patches over her face, neck and lower arms. Dermatological review indicated multiple solar keratoses”. Skin biopsy from the right forearm confirmed this clinical diagnosis – “skin showing hyperkeratosis with a little parakeratosis and acanthosis. The keratinocytes have a glassy appearance but show nuclear atypia with dyskeratotic cells, and occasional suprabasal mitoses. The intraepidermal sweat ducts are spared. Appearances suggest an actinic keratosis with moderate to severe dysplasia.” These features are characteristic of a low grade premalignant change.
She was treated with local 5-fluorouracil cream (Efudix) (3 cycles) to the affected lesions. These photos were taken at the apogee of inflammation. The inflammation resolved after discontinuing the cream. This reaction is expected with application of this mild chemotherapy agent. Alternative or supplementary treatments include cryotherapy, curettage and cautery, if necessary. Following treatment her skin was much softer and considerably improved. Voriconazole has been stopped, and posaconazole substituted.
 ,
,  ,
,  ,
, 




