Date: 26 November 2013
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.
Copyright:
Fungal Research Trust
Notes: n/a
Images library
-
Title
Legend
-
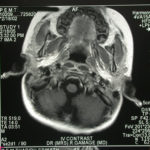
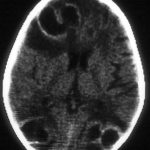
Image a. 3 yr old boy with CNS aspergillosis pt TS. MRI scan pre-amphotericin B
-
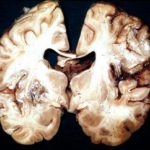
Section though unfixed brain showing large pale area of infarction deep in the parietal cortex, in which Aspergillus hyphae were seen histologically. The patient developed disseminated aspergillosis after a prolonged stay in intensive care after contracting severe community acquired pneumonia.
-
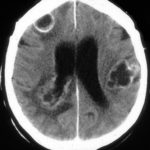
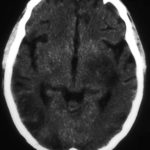
The woman had received a renal transplant several months prior to developing a stroke with reduced consciousness. The enhanced CT scan of her brain showed multiple ring-enhancing lesions bilaterally with little surrounding oedema. Biopsy confirmed invasive aspergillosis on histology and culture.
-
Further details
Image A. Multiple ring enhancing abscesses with substantial surrounding oedema was demonstrated. He had no focal neurological deficits. A needle aspiration confirmed the clinical impression of cerebral aspergillosis by culture and microscopy.
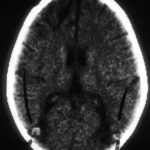
Image B. Resolution of cerebral aspergillosis, pt MN. Focal scars with some surrounding oedema are seen in the site of the prior abscesses.
 ,
, 
-
Contrast enhanced CT scan of the brain showing unequivocally 2 hypodense lesions, one in the left basal ganglia and one in the right occipital cortex. There is the possibility of another smaller left sided occiptal cortex. These lesions do not have the appearance of abscesses, but rather of ischaema.

-
Unenhanced CT scan of the brain in an allogeneic bone marrow transplant recipient demonstrating a large, variably hypodense lesion in the area of the left basal ganglia and possible additional lesions in the posterior parietal and/or occipital cortex.
-
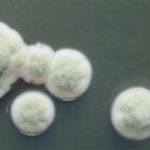
A. versicolor by microscopy showing very long thin conidiophores.

-
Pigmentation of Aspergillus versicolor colonies ranged from pale green to greenish-beige, pink-green, dark green and brown. Reverse is usually reddish. The growth rate is usually slow. Cultured on Sabouraud dextrose agar with chloramphenicol.

-
A Colonies on MEA after one week; B, C conidial heads with tip of conidiophire, x920; D conidial head, x 2330; E conidial heads x920

-
Cultures were grown on malt extract agar. Image kindly provided by Niall Hamilton.