Date: 26 November 2013
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.
Copyright:
Fungal Research Trust
Notes: n/a
Images library
-
Title
Legend
-
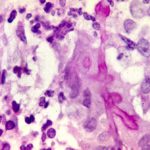
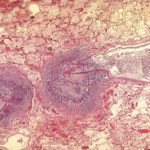
Vascular thrombosis. Medium power view (H&E) of a blood vessel occluded by fungal hyphae and thrombosis. Some fungal hyphae can be seen traversing the vessel wall.

-
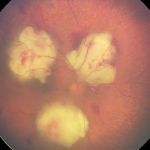
Four colonies of Aspergillus on an agar plate containing rose bengal (to limit colony spending) and elastin fibres (light pink dots). Underneath and surrounding the colonies, the elastin fibres have gone, indicating enzymatic degradation

-
High power view of elastin fibres in an arterial wall being forced apart by Aspergillus hyphae. As Aspergillus is angiotropic and produces an elastase, it was uncertain how it traversed vessel walls. It appears to do so without any dissolution of elastin fibres.

-
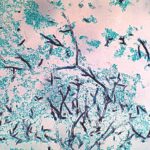
Medium power view (GMS) of hyphae seen within an arterial wall which is characteristic of angioinvasive Aspergillus.

-
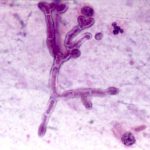
High power view (H&E) of a branching mould, consistent with Aspergillus inside a giant cell in a patient with chronic granulomatous disease.
-
High power view (GMS) of an Aspergillus hypha within a giant cell in a patient with chronic granulomatous disease infected with Aspergillus.

-
Medium power view (GMS) of the contents of a cerebral abscess in which there are hyphae typical of Aspergillus. Aspergillus fumigatus was grown from adjacent tissue.
-
Low power view (H&E) showing a pulmonary vein and a small bronchus infiltrated by fungal hyphae with associated necrotising inflammation.
-
Bilateral A. fumigatus endophthalmitis in association with pulmonary and cerebral aspergillosis, complicating severe autoimmune disease treated with intense immunosuppression. Right eye.