Date: 26 November 2013
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.
Copyright:
Fungal Research Trust
Notes: n/a
Images library
-
Title
Legend
-
Yamik catheter for rinsing nasal and paranasal cavities. Image B

-
Yamik catheter for rinsing nasal and paranasal cavities. Image E
-
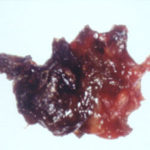
Patient with allergic fungal sinusitis. Eosinophilic mucin with A. flavus in the nasal cavity. Irregular crust of 2.5 cm from a patient diagnosed as allergic fungal sinusitis.
-
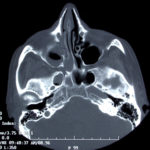
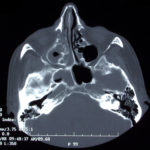
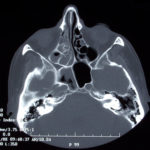
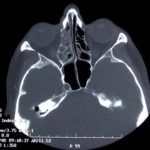
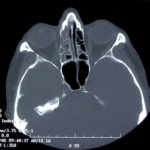
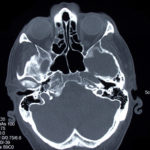
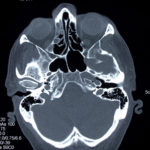
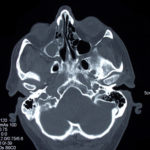
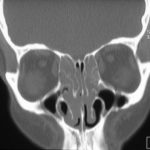
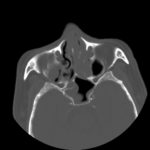
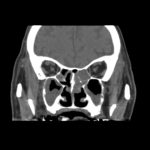
This patient was diagnosed with Myelodyspasia/ Acute Myeloid Leukaemia in January 05. When he received intensive chemotherapy. Had previous history of chronic sinusitis, but after chemotherapy he developed significant maxillary sinusitis. He was treated with Caspofungin with good response, and subsequently with voriconazole. Patient has further CT scans in August 05 with myelodysplasia in remission.
A biopsy of ethmoid sinus in May showed a chronic inflammmatory process with bony invasion by fungal hyphae. The patient was in remission from myelodysplasia and was not undergoing treatment for this at the time of the scans.
In Aug 05 scans show the right maxillary sinus is now opacified. Destruction of superior medial wall of right maxillary sinus. Superiorly there was bone destruction with communication with the lower right ethmoid air cells. Lateral wall of right maxillary sinus remains thick walled with irregular periosteal thickening. No significant abnormality is seen within the nasal cavity or left paranasal sinuses. The biopsy of the ethmoid sinus revealed hyphae consistent with aspergillus. Since the patient was on voriconazole at this time this may indicate resistance. The case is ongoing with further surgery for debridement of right nasal side imminent. The patient is currently in remission.
Feb 06 D Denning
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
, 
-
This 33 year old woman with severe asthma since childhood and recent nasal obstruction, who did not fulfil the criteria for ABPA, had evidence of skin test sensitisation to Aspergillus. Itraconazole therapy orally improved her pulmonary symptoms and allowed a substantial reduction in the need for oral steroids and inhaled steroids. Nasal polyposis improved slightly, but she still required polypectomy and nasal steroids.
 ,
, 
-
Further details
Image A. The bone appears normal, but the features are most consistent with infection, less so with a pseudotumour. Bone windows not shown. Biopsy demonstrated hyphal invasion and cultures grew A. fumigatus.
 ,
,  ,
,  ,
, 



 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,