Date: 26 November 2013
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.
Copyright:
Fungal Research Trust
Notes: n/a
Images library
-
Title
Legend
-
Facial erythema: Voriconazole rash in ABPA patient resistant to corticosteroids, treated with voriconazole 200mg BID. Serum voriconazole levels were very low and the dose was raised to 250mg BID. Within 3 weeks patient had developed remarkable facial erythema. His trough voriconazole concentration at this time was 370ng/ml. When voriconazole was stopped because of the facial erythema and lack of impact on his ABPA his facial erythema resolved over 4 weeks.
Forearm erythema related to voriconazole. As with facial erythema patient developed remarkable forearm erythema with lesions similar to porphyria cutanea tarda all of which resolved with stopping voriconazole.
 ,
,  ,
, 
-
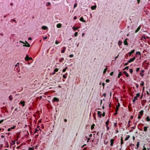
Eosinophilic mucin containing numerous eosinophils and Charcot-Leyden crystals (arrow). Stain PAS x400. Patient with allergic fungal sinusitis
-
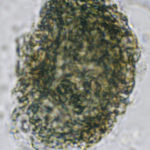
A whole fungal ball removed from the sinus by endoscopic surgery. No staining x 10
-
Crushed fungal material removed from sinus by endoscope. No staining x40

-
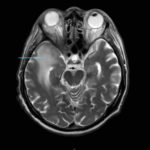
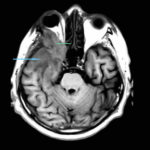
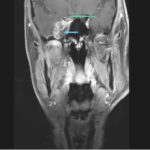
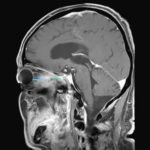
This 68 year man with a history of hypertension and ischemic heart disease presented with nasal obstruction, localised swelling and pain in his right cheek for about two months. CT scan showed a soft tissue mass filling the right maxillary sinus adjacent to the floor of the orbit. Maxillotomy with mass removal was performed and culture grew A. fumigatus. Histology was not performed and the patient received no antifungal therapy. 5 months later localised relapse with progression along the medial wall of the orbit was seen on CT scan.
 ,
,  ,
,  ,
,  ,
,  ,
, 
-
Yamik catheter for rinsing nasal and paranasal cavities. Image D

-
Yamik catheter for rinsing nasal and paranasal cavities. Image C





