Date: 26 November 2013
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.
Copyright:
Fungal Research Trust
Notes: n/a
Images library
-
Title
Legend
-
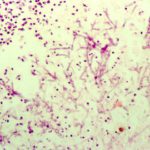
Pulmonary aspergillosis (K&E) (parrot C). Tissue from an individually housed and recently purchased, 6 month old African grey parrot found dead in the cage. Necropsy examination revealed focal necrosis of the left lung. This section stained by haematoxylin and eosin reveals septate fungal hyphae within the lung parenchyma. Similar hyphae were located in the walls and lumen of parabronchi, and within the walls of pulmonary blood vessels.

-
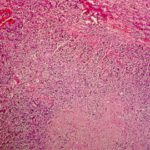
Nasal aspergillosis. Tissue from an 8 year old, neutered male thoroughbred horse with an initial history of sinusitis leading to progressive neurological signs (ataxia, behavioural abnormalities) and prolonged recumbency. Necropsy examination revealed a focus of grey-caseous material within the right nasal chamber that comprised a mat of branching, septae fungal hyphae and mixed inflammatory cells (haematoxylin and eosin stain). Aspergillus spp was cultured from the lesion. There was no gross or histologica
-
Immunofluorescence. Section of renal granuloma from dog J stained with polyclonal antiserum specific for Aspergillus terreus by immunofluorescence.

-
Complement deposition (dog J). Section of myocardial granuloma from dog J stained for canine complement C3 by immunofluorescence. Deposition of C3, but not C4, on fungal hyphae suggests activation of the alternative rather than classical pathway of complement.

-
Lymph node granuloma – Section of lymph node granuloma from a German shepherd dog with disseminated aspergillosis stained for canine IgA by immunofluorescence. The fungal hyphae within the centre of the lesion have surface IgA, and IgA-bearing plasma cells are present within the surrounding inflammatory infiltrate

-
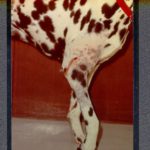
Extensive focus of pyogranulomatous inflammation within the kidney of dog J
-
Aspergillus granuloma within the myocardium of dog J.

-
Retinal aspergillosis (dog J) – Section of retina from a German shepherd dog with disseminated aspergillosis. Fungal hyphae and inflammatory cells are found within the vitreous

-
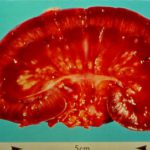
Saggital section of kidney from a German shepherd dog with disseminated aspergillosis. There are granulomata within the medulla, and fungal material within the renal pelvis. Renal involvement in canine dissemianted aspergillosis is common, and the demonstration of fungal hyphae within urine sediment is a useful screening test.