Date: 23 January 2014
A 43 year old with smoking related emphysema was admitted to hospital with two separate episodes of haemoptysis. He had been in good health up to 1989, when he was diagnosed as having bilateral pulmonary tuberculosis. At that time a CT scan revealed a cavity in the left upper lobe (20.8cm2) with adjacent confluent infiltrates and pleural thickening. On bronchoscopic examination no abnormalities were noted and endobronchial biopsies did not reveal hyphae.
Over the next 4 years his condition deteriorated and a CT scan showed the left upper lobe cavity had increased to 40cm2. Itraconazole 400mg daily was prescribed. There was some clinical improvement on itraconazole but patient eventually deteriorated with breathlessness and with significant weight loss.
Copyright: n/a
Notes:
Images library
-
Title
Legend
-
4 Total obstruction of the sinuses due to inflamed mucosa. (Patient 04)
-
1 Axial computed tomography (CT) scans of the frontal sinus.
A: due to the long lasting pressure of mucus, the bone of the anterior wall of frontal sinus is thinned out and elevated anteriorly, forming a bulge. B: same situation as depicted in fig A: the posterior bony wall of frontal sinus is thinned out and extremely elevated posteriorly towards the frontal lobe of the brain. As depicted on the scan, a thin bony layer covering the dura could be recognized intraoperatively
-
2 Same patient as 1 and 3, frontal CT

-
D. 6 months later, tenacious yellow secretions in L basal bronchial division
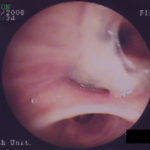
-
C. After suction the material was seen to extend distally – obstructing the right basal stem bronchus

-
B. After suction the material was seen to extend distally – obstructing the right basal stem bronchus