Date: 23 January 2014
A 43 year old with smoking related emphysema was admitted to hospital with two separate episodes of haemoptysis. He had been in good health up to 1989, when he was diagnosed as having bilateral pulmonary tuberculosis. At that time a CT scan revealed a cavity in the left upper lobe (20.8cm2) with adjacent confluent infiltrates and pleural thickening. On bronchoscopic examination no abnormalities were noted and endobronchial biopsies did not reveal hyphae.
Over the next 4 years his condition deteriorated and a CT scan showed the left upper lobe cavity had increased to 40cm2. Itraconazole 400mg daily was prescribed. There was some clinical improvement on itraconazole but patient eventually deteriorated with breathlessness and with significant weight loss.
Copyright: n/a
Notes:
Images library
-
Title
Legend
-
Pt FT. Autopsy appearance of the trachea, after the adherent pseudomembrane had been removed, revealing confluent ulceration superiorly with small green plaques of Aspergillus growth on the trachea inferiorly.

-
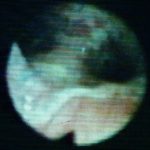
This view was obtained in a lung transplant recipient at bronchoscopy. Aspergillus fumigatus was grown from bronchial lavage but invasion was not demonstrated on bronchial biopsy. Symptoms improved with itraconazole therapy and abnormal appearances had resolved within 2 weeks.

-
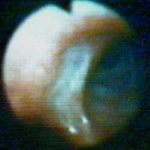
Bronchoscopic view of Aspergillus tracheobronchitis. Bronchial lavage revealed hyphae in microscopy and cultures grew A.fumigatus. This man had received a lung transplant a few weeks before. Invasion of mucosa, but not cartilage, was demonstrated histologically. He responded rapidly to oral itraconazole.
-
This view from indirect laryngoscopy illustrates bilateral lesions on the larynx that on biopsy were shown to be due to Aspergillus. This is a rare disease in non-immunocompromised patients.

-
Bronchoscopic view of a deep bronchial ulcer in a lung transplant patient. Biopsies through the ulcer yielded cartilage with hyphae invading it. Fungal cultures of bronchial lavage grew Aspergillus fumigatus. He responded to oral itraconazole therapy.
-
Patient had life threatening pneumonia, cavity formation was later observed. He later presented with a fungal ball. The aspergilloma was removed by surgical resection of the right upper lobe.
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,