Date: 26 November 2013
Further details
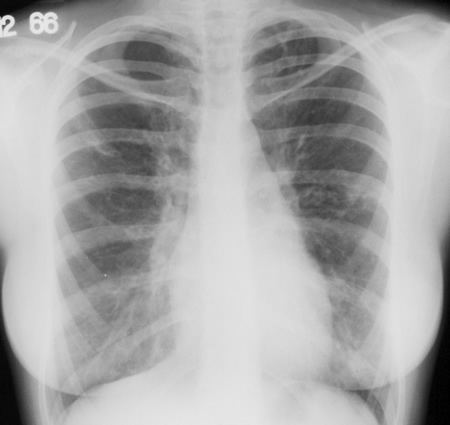
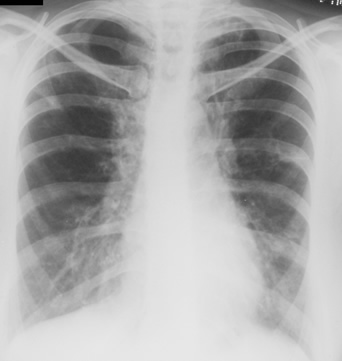
Image A 13/12/66 Asthma. Chest x-ray showing slightly streaky shadowing both bases and left mid and upper zone shadowing, and left apical scarring. The bronchial wall thickening in the left lobe is suspicious of bronchiectasis.
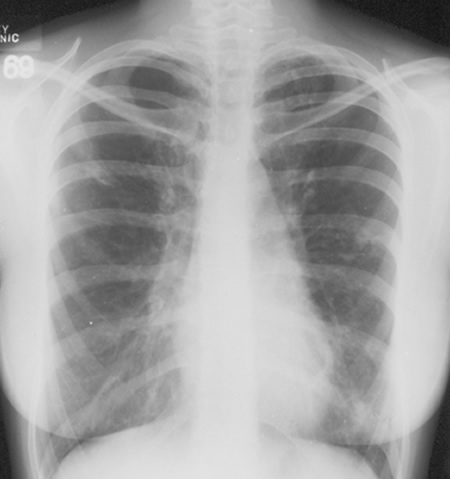
Image B 4/3/69Asthma with bronchiectasis. Chest x-ray showing mild left mid zone shadows consistent with bronchiectasis and a small area of opacification in the left base, with left apical scarring. New streaky shadowing is projected over the left heart border.
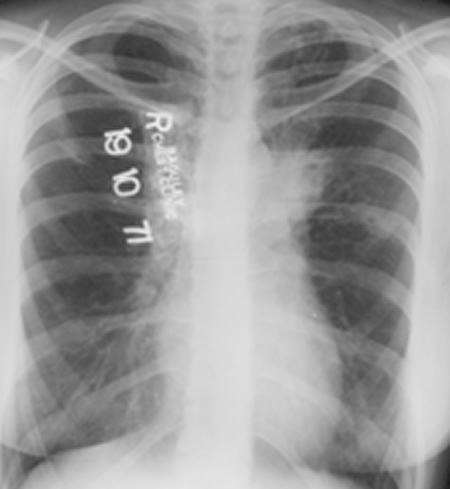
Image C 19/10/71 Asthma with bronchiectasis.Chest x-ray showing obliteration of the left aorto-pulmonary window and upper lobe streaking and cavitation and a mid zone small cavitary lesion, most likely a thickened bronchus end on.
Image D 22/9/81 Asthma with bronchiectasis and first radiological clue of ABPA. Chest x-ray showing left upper zone patchy shadowing or atelectasis with obliteration of the left aorto-pulmonary window. There is new right upper lobe streaky shadowing with slight right upper lobe volume loss.
Image E 3/11/81 Asthma with bronchiectasis and first radiological clue of ABPA. Chest x-ray showing clearance of the left upper lobe shadowing after physiotherapy and corticosteroids, compare with X ray D. This clearing with steroids is characteristic of ABPA. However, there is now extensive bronchiectasis in the left lower and right lower lobes.
Image F 17/9/85 Asthma with bronchiectasis and ABPA, with first clue of chronic cavitary pulmonary aspergillosis (CCPA). Chest x-ray showing development of right upper pleural thickening with further volume loss, without extensive fibrotic disease. There is more obvious new cavity formation in the left upper lobe with unchanged thickened bronchi in the left mid zone. A mild scoliosis has developed.
Image G 19/7/93 Asthma with bronchiectasis and ABPA, with now overt chronic cavitary pulmonary aspergillosis (CCPA), bilaterally Chest x-ray showing extensive shadowing at the right base consistent with a chest infection or plugging, ring shadows and coarse markings throughout the lung fields consistent with bronchiectasis and right apical pleural thickening which has progressed. The cavities in the left upper lobe have expanded in size. Her scoliosis has progressed.
Image H 05/06/95 Asthma with bronchiectasis, ABPA and CCPA with possible airway plugging due to ABPA. Chest x-ray showing interval development of scoliosis with bilateral upper lobe pleural thickening, worse on the right, with cavities in the left upper lobe and fullness of the right upper mediastinum.
Image I 08/03/99 Asthma with bronchiectasis, ABPA and CCPA with obvious progression of bronchiectasis, and ? ABPA-related collapse left side Chest x-ray showing marked scoliosis, stable mild left upper lobe fibrosis and cavity formation, and stable right upper lobe pleural thickening. Her trachea is newly displaced to the right. There is a rounded peripheral wedge-shaped area in the right upper lobe, possibly sub-segmental collapse. Both cystic and varicose bronchiectasis are seen in the proximal left lower lobe.
Image J 11/10/02 Asthma with bronchiectasis, ABPA and CCPA which has progressed. Chest x-ray ( computed radiography) showing extensive bronchiectasis, with contraction and fibrosis with cavitation of the left apex, right upper pleural thickening also with cavities in the right upper zone. Large cavities are seen immediately to the right of the trachea with a probable fluid level.
Image K 05/04/04 Asthma with bronchiectasis, ABPA and CCPA with large airway disease of uncertain cause. Chest radiograph showing a right apical cavity free of fluid. Possible constriction of the trachea above the carina and also of the proximal left main bronchus, without an obvious extrinsic mass. There is some improvement of the right upper lobe pleural thickening inferiorly. Otherwise other findings are stable.
Image L. Case MD (now aged 67). In late 2005, she deteriorated on itraconazole and was admitted to hospital for antibiotic therapy. Coughing resulted in a rib fracture. Her prednisolone dose was 10mg daily, necessary to control her asthma and respiratory symptoms, but had lead to osteoporosis and an achilles tendon rupture. Her total IgE was 910KIU/L in August 2005, and Aspergillus specific IgE 34.4 KUa/L, lower than some years before. Pseudomonas was being grown continually from her sputum. Her symptoms continued despite antibiotics and it was judged that her ABPA was out of control, and voriconazole 200mg twice daily was substituted, and itraconazole stopped.
Over the following months and years, there was gradual improvement in her chest symptoms. Her prednisolone dose was reduced to 5mg daily, and given in combination with a moderate dose inhaled steroid. Her total IgE fell to 310 KIU/L and Aspergillus specific IgE to 9.0 KUa/L by 2009. Her FEV1 and FVC had remained stable between 1999 and 2010 at 0.95 and 2.04 (pre-salbutamol) and 1.0 and 2.29.
She had one admission for a chest infection requiring antibiotics in 2011. Her walking distance once she had recovered was 150 meters and her FEV1 in 2011 was 0.82. She continued to remain well and at the end of 2014 was still colonised by Pseudomonas, but doing well. Her XR was almost unchanged from 2004.
Copyright:
Kindly supplied by David Denning
Notes: n/a
Images library
-
Title
Legend
-
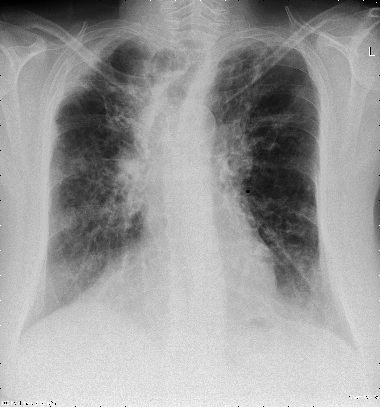
The chest X rays showed a rapid progression of lung disease- with bilateral upper zone and midzone consolidation and bilateral pleural effusion. Both lower lobes showed bronchiectasis in a central distribution along with centrilobular nodules and tree-in-bud pattern.
 ,
,  ,
,  ,
, 
-
Patient EG Intraluminal aspergilloma in cystic fibrosis (12 months follow up)
The 21 year old woman with cystic fibrosis developed an aspergilloma in her left lower lobe bronchus. CF was diagnosed at 6 months of age (sweat chloride 78 and 100 mmol/L) and CFTR mutations δ508 and W1282X and she developed diabetes mellitus at age 12 years. Age 15 years ABPA was diagnosed. Her serum IgE at the time of diagnosis was 5060 IU/L, skin prick test for aspergillus was positive, and serum was positive for precipitating antibodies to Aspergillus. She was treated with oral prednisone (1 mg/kg/day) for first two weeks followed by prednisone at 0.5 mg/kg every other day for at least 6 months with some clinical and serologic improvement. Over the following 5 years, she presented with a pattern of repeated episodic exacerbations with wheezing and crackles, increases in IgE and need to increase prednisone dosage.
In the 12 months before the aspergillomas were found, she started to experience frequent pulmonary exacerbations, which have prompted intensive therapies. She has also been on oral prednisone & itraconazole for at least 9 months for her ABPA relapse with some clinical & serologic improvement. She then developed severe protracted coughing spells associated with minor hemoptysis, low grade intermittent fever, and weight loss. Her FEV1 declined in a 3 months period from 56% to 33%. A recent chest-x ray did not reveal any new changes when compared to the one obtained almost a year before. A CT scan of the chest, however shows an ovoid soft tissue density within an ectatic bronchi in the anterior basal segment of the lower left lobe, felt to be an aspergilloma. [Link here].
She was started on voriconazole 200 mg twice daily. This dose gave a random serum level of 5ug/L. Her prednisone was weaned to 5 mgs/day and her FEV1 increased to 46% of predicted. In January 2009, her IgE level was 3053 kU/L; one year later, her IgE level was 1167 kU/L. A lung transplant surgeon attempted unsuccessfully to remove the aspergilloma via flexible bronchoscopy. It took a while for her to recover from that procedure. She then had a pulmonary exacerbation. She tolerated voriconazole reasonably well and gaining some weight. By mid 2010, her IgE level was 637 IU/L.
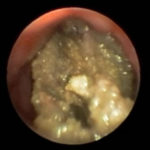
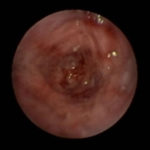
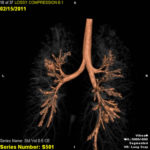
In early 2011, her aspergilloma (yellow friable material) in the anterior segment of the left lower lobe was removed completely (Fig a and b). It took a little time, but with biopsy forceps and some mincing and homogenization, it was all sucked out. The 3D reconstruction (Fig c) only shows the area of bronchiectasis, not the aspergilloma.Dr. Turcios is the director of pediatric pulmonology/cystic fibrosis in Somerville, NJ.
 ,
,  ,
, 
-
This patient is a 70 yr old, obese diabetic with aortic stenosis and COPD. He was admitted in early March 09, with collapse and loss of conciousness. His lungs appeared normal at this time – CT and X-ray 1. 10 days later he was admitted with increasing shortness of breath and chest X ray (F) showing widespread patchy consolidation. CT scan (B) showed bronchial dilatation, mucus plugging, nodular and bibasal consolidation. Multiple sputum samples grew Aspergillus fumigatus. The patient required intubation and remained in ITU for 160 days.
Bronchoscopy showed plaques in the major airways with more distal airways plugged with secretions resembling “cottage cheese”.There was severe contact bleeding and oedematous mucosa (I & J). Biopsy of the plaques showed fungal hyphae with a branching pattern consistent with aspergillus infection (G & H).
The patient was initially given IV and nebulised amphotericin B whilst on doses of hydrocortisone from 100-400 mg/day. Voriconazole was added with dose optimisation, and amphotericin discontinued. The patient improved gradually with voriconazole treatment over several months and for the latter month, gamma interferon was added into his regime which further improved his CT scan although some shadowing and bronchial wall thickening was still seen (D).
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
, 
-
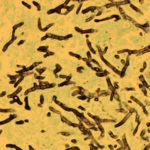
Hyphal septate club-like enlargements from culture on CYA 25°C medium (mag x100)

-
G Potassium hydroxide preparation of a nail specimen with onychomycosis- examined by microscopy