Date: 26 November 2013
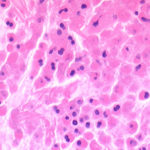
This patient with ABPA and chronic cavitary pulmonary aspergillosis has been stabilized on voriconazole treatment for >5 years. She had a degree of photosensitivity most of that time, noticed early in the course of voriconazole treatment. She is oxygen and wheelchair dependent and doesn’t go outside very much, so most of her light exposure has been indoor light. She developed rough scaly patches over her face, neck and lower arms. Dermatological review indicated multiple solar keratoses”. Skin biopsy from the right forearm confirmed this clinical diagnosis – “skin showing hyperkeratosis with a little parakeratosis and acanthosis. The keratinocytes have a glassy appearance but show nuclear atypia with dyskeratotic cells, and occasional suprabasal mitoses. The intraepidermal sweat ducts are spared. Appearances suggest an actinic keratosis with moderate to severe dysplasia.” These features are characteristic of a low grade premalignant change.
She was treated with local 5-fluorouracil cream (Efudix) (3 cycles) to the affected lesions. These photos were taken at the apogee of inflammation. The inflammation resolved after discontinuing the cream. This reaction is expected with application of this mild chemotherapy agent. Alternative or supplementary treatments include cryotherapy, curettage and cautery, if necessary. Following treatment her skin was much softer and considerably improved. Voriconazole has been stopped, and posaconazole substituted.
Copyright:
DW Denning and JE Ferguson, University Hospital of South Manchester. 22/07/08
Notes: n/a
Images library
-
Title
Legend
-
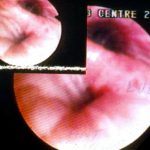
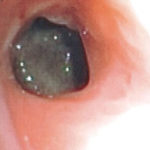
A. Necrotic mass prolapsing in and out of the distal right intermediate bronchus obscuring both the basal stem and basal division

-
History : A 20 yr old female with cystic fibrosis complicated by CF-related Diabetes mellitus (diagnosed at age 12 years) & ABPA (diagnosed at
15 years ). She was fairly stable until last 9 months, when she started to experience frequent pulmonary exacerbations, which have prompted intensive therapies.
Her serum IgE at the time of diagnosis was 5060 IU/L, skin prick test for aspergillus was positive, and serum was positive for precipitating antibodies to Aspergillus. She was treated with oral prednisone (1 mg/kg/day) for first two weeks followed by prednisone at 0.5 mg/kg every other day for at least 6 months with some clinical and serologic improvement. Over the following 5 years, she presented with a pattern of repeated episodic exacerbations with wheezing and crackles, increases in IgE and need to increase prednisone dosage. In an attempt to control her frequent ABPA relapses, itraconazole was added at 200mg twice a day, with some clinical & serologic improvement.
2-3 weeks prior to the scans and X rays, she developed severe protracted coughing spells associated with minor hemoptysis, low grade intermittent fever, and weight loss. Her FEV1 declined in a 3 months period from 56% to 33%.
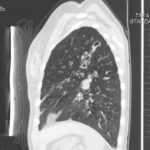
A chest-x ray (Fig 3) did not reveal any new changes when compared to the one obtained almost a year before. A CT scan of the chest Figs 1 and 2- lateral view), however shows an ovoid soft tissue density within an ectatic bronchi in the anterior basal segment of the LLL, felt to be an aspergilloma.She was started on oral voriconazole (3 months after the above scans and X-rays) which is better absorbed in CF patients than itraconazole, at 200mg twice a day. Her prednisone was gradually reduced to 5 mgs/day and her FEV1 increased to 46% of predicted (03/31/10), her IgE level was 1167 kU/L (previously in January 2009, her IgE level was 3053 kU/L)and her weight has plateaued.
Since she was not fit enough for surgery at that time, removing the aspergilloma by flexible bronchoscopy was unsuccessful. The aspergilloma can be seen at bronchoscopy in Fig 4. ,
,  ,
,  ,
, 
-
Widespread mucoid impaction also seen, particularly in left side, suggestive of allergic bronchopulmonary aspergillosis.

-
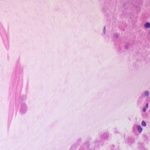
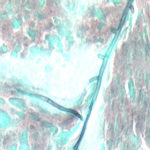
Microscopy of fungal hyphae isolated from fungal culture (lactophenol blue)
-
A CT scan performed at this time showed an enhancing lesion with ill defined margins involving the pterigopalatine fossa, the maxillary antrum , orbital apex and middle cranial fossa. There was also destruction of boney architecture locally.
-
The patient underwent a pneumonectomy because of the severity of her disease process, and uncertainty about the diagnosis, prior to serology results being obtained.
Serology showed an IgE of 2600, with a strongly positive Aspergillus RAST test and weakly positive Aspergillus precipitins. Material removed at bronchoscopy showed eosinophilia. These features confirm a diagnosis of allergic bronchopulmonary aspergillosis (ABPA).
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
, 






 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,