Date: 26 November 2013
This patient with ABPA and chronic cavitary pulmonary aspergillosis has been stabilized on voriconazole treatment for >5 years. She had a degree of photosensitivity most of that time, noticed early in the course of voriconazole treatment. She is oxygen and wheelchair dependent and doesn’t go outside very much, so most of her light exposure has been indoor light. She developed rough scaly patches over her face, neck and lower arms. Dermatological review indicated multiple solar keratoses”. Skin biopsy from the right forearm confirmed this clinical diagnosis – “skin showing hyperkeratosis with a little parakeratosis and acanthosis. The keratinocytes have a glassy appearance but show nuclear atypia with dyskeratotic cells, and occasional suprabasal mitoses. The intraepidermal sweat ducts are spared. Appearances suggest an actinic keratosis with moderate to severe dysplasia.” These features are characteristic of a low grade premalignant change.
She was treated with local 5-fluorouracil cream (Efudix) (3 cycles) to the affected lesions. These photos were taken at the apogee of inflammation. The inflammation resolved after discontinuing the cream. This reaction is expected with application of this mild chemotherapy agent. Alternative or supplementary treatments include cryotherapy, curettage and cautery, if necessary. Following treatment her skin was much softer and considerably improved. Voriconazole has been stopped, and posaconazole substituted.
Copyright:
DW Denning and JE Ferguson, University Hospital of South Manchester. 22/07/08
Notes: n/a
Images library
-
Title
Legend
-
This 24-year-old male with AML on chemotherapy developed recent onset fever and cough. B- Representative section of High Resolution CT shows centri-lobular nodules, ‘tree-in-bud’ appearance consistent with bronchogenic spread of disease.

-
This 24-year-old male with AML on chemotherapy developed recent onset fever and cough. A: Chest radiograph showing patchy air space consolidation involving both lungs.

-
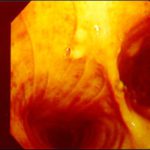
This man with severe chronic fibrosing alveolitis underwent a single left lung transplant at the end of November 2004. Postoperatively he developed reperfusion pulmonary oedema and was difficult to ventilate. He also developed acute renal failure requiring haemodialysis/haemofiltration which corrected his fluid overload and rising creatinine.Rejection was prevented with cyclosporin, mycophenolate and a decreasing dose of methylprednisolone. Cardiovascular problems identified mild pulmonary anastomostic stenosis with a 5% pressure gradient. He had a tracheostomy about 12 days post transplant. He then developed episodes of hypoxia and increased ventilatory pressures. Several bronchoscopies showed mucus plugging in the trachea and major bronchi. These were aspirated, with improvement of oxygenation. Cultures of one of these plugs grew A. fumigatus. These images show a bronchoscopy view of the trachea and anastomosis. Major obstruction of the airway is visible (70%) distal to the anastomosis which looks healthy. Some evidence of tracheal inflammation is visible.
 ,
, 
-
The chest x-ray shows a patient who had a left lung transplanted in May 2003 for cryptogenic fibrosing alveolitis, which was diagnosed post-transplant as sarcoidosis.

-
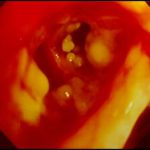
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.

-
Tracheal aspergillosis, Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.

-
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.
-
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.
-
Aspergillus tracheobronchitis in a normal child. This figure, drawn in 1890, illustrates the appearances of the trachea and main bronchi at autopsy in a 3 year old child. She had little else wrong at autopsy other than a minor degree of tuberculosis. She is the first recorded case of Aspergillus tracheobronchitis in the literature and illustrates well that this disease can affect previously well non-inimmunocompromised people. The full case is reported in Wheaton SW.

-
pt FT. Normal chest radiograph of patient with extensive pseudomembranous Aspergillus tracheobronchitis, 4 days before death.





