Date: 26 November 2013
This patient with ABPA and chronic cavitary pulmonary aspergillosis has been stabilized on voriconazole treatment for >5 years. She had a degree of photosensitivity most of that time, noticed early in the course of voriconazole treatment. She is oxygen and wheelchair dependent and doesn’t go outside very much, so most of her light exposure has been indoor light. She developed rough scaly patches over her face, neck and lower arms. Dermatological review indicated multiple solar keratoses”. Skin biopsy from the right forearm confirmed this clinical diagnosis – “skin showing hyperkeratosis with a little parakeratosis and acanthosis. The keratinocytes have a glassy appearance but show nuclear atypia with dyskeratotic cells, and occasional suprabasal mitoses. The intraepidermal sweat ducts are spared. Appearances suggest an actinic keratosis with moderate to severe dysplasia.” These features are characteristic of a low grade premalignant change.
She was treated with local 5-fluorouracil cream (Efudix) (3 cycles) to the affected lesions. These photos were taken at the apogee of inflammation. The inflammation resolved after discontinuing the cream. This reaction is expected with application of this mild chemotherapy agent. Alternative or supplementary treatments include cryotherapy, curettage and cautery, if necessary. Following treatment her skin was much softer and considerably improved. Voriconazole has been stopped, and posaconazole substituted.
Copyright:
DW Denning and JE Ferguson, University Hospital of South Manchester. 22/07/08
Notes: n/a
Images library
-
Title
Legend
-
Itraconazole rash – macropopular rash after 7 days treatment with Itraconazole, in a patient with AIDS

-
A 72 year-old male patient had been in treatment for many years for severe asthma with relatively good exercise tolerance. Over the past two years he had increasing problems of shortness of breath, cough and productive sputum. There was no history of chest pain, haemoptysis or fever. His total IgE was 680.0 IU/l, and specific IgE against Aspergillus fumigatus was 14.6 IU/l. Precipitins against A. fumigatus were weakly positive (titre 1/2), and there was no eosinophilia. Computed tomography revealed marked emphysema but only mild bronchiectasis. Based on these results he was diagnosed with severe asthma with fungal sensitisation (SAFS) and itraconazole was started (SporanoxTM 200mg bds). Itraconazole dosage was reduced to 200 mg daily one month later due to progressive bilateral ankle oedema. Itraconazole levels by bioassay were 17.5 mg/l at that time (normal range 5-15 mg/l). Despite showing improvement on his chest symptoms, peripheral oedema became a major negative impact on patient’s quality of life. There were no signs of heart failure. Figure 1 was taken 2 months after itraconazole was started, when drug levels were 9.8 mg/l. Itraconazole was replaced by voriconazole. Concomitant medications included furosemide (80 mg daily) and spironolactone (100 mg daily). After discontinuing itraconazole, the oedema quickly subsided.
Ankle oedema is an uncommon complication of therapy with itraconazole. It has occurred in about 4% of patients treated in clinical trials involving this drug. This complication seems to be more frequent in patients concomitantly receiving calcium channel blockers, which was not the case for our patient. The mechanism is unknown. It usually does not represent cardiac failure, another reported side effect of itraconazole, but this must be excluded. Marked oedema requiring drug suspension is a rare phenomenon, and has not been previously reported in association with itraconazole.
 ,
,  ,
, 
-
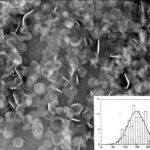
The insert shows the size of the discs. These discs dissociate after infusion to release amphotericin B preferentially into the reticuloendothelial system and lung. This form of amphotericin B is marketed as either Amphotec or Amphocil, depending on the country.