Date: 26 November 2013
This patient with ABPA and chronic cavitary pulmonary aspergillosis has been stabilized on voriconazole treatment for >5 years. She had a degree of photosensitivity most of that time, noticed early in the course of voriconazole treatment. She is oxygen and wheelchair dependent and doesn’t go outside very much, so most of her light exposure has been indoor light. She developed rough scaly patches over her face, neck and lower arms. Dermatological review indicated multiple solar keratoses”. Skin biopsy from the right forearm confirmed this clinical diagnosis – “skin showing hyperkeratosis with a little parakeratosis and acanthosis. The keratinocytes have a glassy appearance but show nuclear atypia with dyskeratotic cells, and occasional suprabasal mitoses. The intraepidermal sweat ducts are spared. Appearances suggest an actinic keratosis with moderate to severe dysplasia.” These features are characteristic of a low grade premalignant change.
She was treated with local 5-fluorouracil cream (Efudix) (3 cycles) to the affected lesions. These photos were taken at the apogee of inflammation. The inflammation resolved after discontinuing the cream. This reaction is expected with application of this mild chemotherapy agent. Alternative or supplementary treatments include cryotherapy, curettage and cautery, if necessary. Following treatment her skin was much softer and considerably improved. Voriconazole has been stopped, and posaconazole substituted.
Copyright:
DW Denning and JE Ferguson, University Hospital of South Manchester. 22/07/08
Notes: n/a
Images library
-
Title
Legend
-
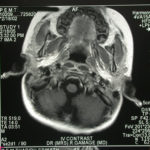
Image b. 3 yr old boy with CNS aspergillosis pt TS. MRI scan pre-amphotericin B.

-
Image a. 3 yr old boy with CNS aspergillosis pt TS. MRI scan pre-amphotericin B
-
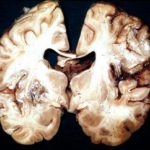
Section though unfixed brain showing large pale area of infarction deep in the parietal cortex, in which Aspergillus hyphae were seen histologically. The patient developed disseminated aspergillosis after a prolonged stay in intensive care after contracting severe community acquired pneumonia.
-
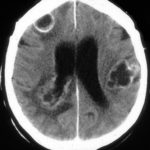
The woman had received a renal transplant several months prior to developing a stroke with reduced consciousness. The enhanced CT scan of her brain showed multiple ring-enhancing lesions bilaterally with little surrounding oedema. Biopsy confirmed invasive aspergillosis on histology and culture.
-
Further details
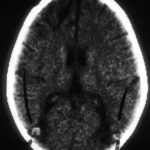
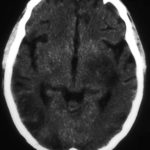
Image A. Multiple ring enhancing abscesses with substantial surrounding oedema was demonstrated. He had no focal neurological deficits. A needle aspiration confirmed the clinical impression of cerebral aspergillosis by culture and microscopy.
Image B. Resolution of cerebral aspergillosis, pt MN. Focal scars with some surrounding oedema are seen in the site of the prior abscesses.
 ,
, 
-
Contrast enhanced CT scan of the brain showing unequivocally 2 hypodense lesions, one in the left basal ganglia and one in the right occipital cortex. There is the possibility of another smaller left sided occiptal cortex. These lesions do not have the appearance of abscesses, but rather of ischaema.

-
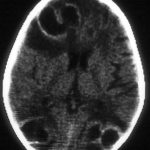
Unenhanced CT scan of the brain in an allogeneic bone marrow transplant recipient demonstrating a large, variably hypodense lesion in the area of the left basal ganglia and possible additional lesions in the posterior parietal and/or occipital cortex.
-
A. versicolor by microscopy showing very long thin conidiophores.

-
Pigmentation of Aspergillus versicolor colonies ranged from pale green to greenish-beige, pink-green, dark green and brown. Reverse is usually reddish. The growth rate is usually slow. Cultured on Sabouraud dextrose agar with chloramphenicol.

-
A Colonies on MEA after one week; B, C conidial heads with tip of conidiophire, x920; D conidial head, x 2330; E conidial heads x920





