Date: 26 November 2013
This patient with ABPA and chronic cavitary pulmonary aspergillosis has been stabilized on voriconazole treatment for >5 years. She had a degree of photosensitivity most of that time, noticed early in the course of voriconazole treatment. She is oxygen and wheelchair dependent and doesn’t go outside very much, so most of her light exposure has been indoor light. She developed rough scaly patches over her face, neck and lower arms. Dermatological review indicated multiple solar keratoses”. Skin biopsy from the right forearm confirmed this clinical diagnosis – “skin showing hyperkeratosis with a little parakeratosis and acanthosis. The keratinocytes have a glassy appearance but show nuclear atypia with dyskeratotic cells, and occasional suprabasal mitoses. The intraepidermal sweat ducts are spared. Appearances suggest an actinic keratosis with moderate to severe dysplasia.” These features are characteristic of a low grade premalignant change.
She was treated with local 5-fluorouracil cream (Efudix) (3 cycles) to the affected lesions. These photos were taken at the apogee of inflammation. The inflammation resolved after discontinuing the cream. This reaction is expected with application of this mild chemotherapy agent. Alternative or supplementary treatments include cryotherapy, curettage and cautery, if necessary. Following treatment her skin was much softer and considerably improved. Voriconazole has been stopped, and posaconazole substituted.
Copyright:
DW Denning and JE Ferguson, University Hospital of South Manchester. 22/07/08
Notes: n/a
Images library
-
Title
Legend
-
Facial erythema: Voriconazole rash in ABPA patient resistant to corticosteroids, treated with voriconazole 200mg BID. Serum voriconazole levels were very low and the dose was raised to 250mg BID. Within 3 weeks patient had developed remarkable facial erythema. His trough voriconazole concentration at this time was 370ng/ml. When voriconazole was stopped because of the facial erythema and lack of impact on his ABPA his facial erythema resolved over 4 weeks.
Forearm erythema related to voriconazole. As with facial erythema patient developed remarkable forearm erythema with lesions similar to porphyria cutanea tarda all of which resolved with stopping voriconazole.
 ,
,  ,
, 
-
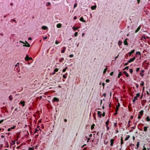
Eosinophilic mucin containing numerous eosinophils and Charcot-Leyden crystals (arrow). Stain PAS x400. Patient with allergic fungal sinusitis
-
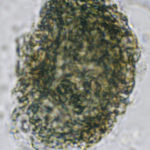
A whole fungal ball removed from the sinus by endoscopic surgery. No staining x 10
-
Crushed fungal material removed from sinus by endoscope. No staining x40

-
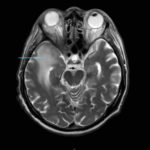
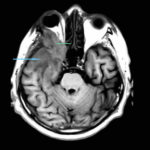
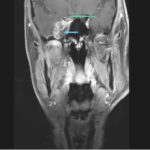
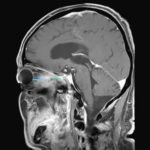
This 68 year man with a history of hypertension and ischemic heart disease presented with nasal obstruction, localised swelling and pain in his right cheek for about two months. CT scan showed a soft tissue mass filling the right maxillary sinus adjacent to the floor of the orbit. Maxillotomy with mass removal was performed and culture grew A. fumigatus. Histology was not performed and the patient received no antifungal therapy. 5 months later localised relapse with progression along the medial wall of the orbit was seen on CT scan.
 ,
,  ,
,  ,
,  ,
,  ,
, 
-
Yamik catheter for rinsing nasal and paranasal cavities. Image D









