Date: 26 November 2013
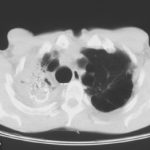
The patient was a 37-year old man in whom P.carinii pneumonia developed in August 1987, followed by esophageal candidiasis and upper gastrointestinal bleeding in September. Chronic perineal herpes led to the formation of rectourethral fistula and multiple episodes of urosepsis, for which he was given long-term ciprofloxacin therapy to suppress bacterial colonization of the bladder. He discontinued heavy alcohol use in September 1987 and smoked marijuana occasionally.On April 23 1989, the patient was admitted to the hospital with a two-month history of increasing dry cough with shortness of breath. He reported transient fever (temperature to 41°C). He was admitted with leukopenia, with his neutrophil count falling to 16 x 106/l on the second hospital day. A chest film showed bilateral fluffy lower-lobe infiltrates (this image). Zidovudine was discontinued. The patient had a rapidly downhill course despite intravenous treatment with trimethioprim-sulfamethoxazole. A bronchoscopy on the sixth hospital day revealed what appeared to be a foreign body in the left lower-lobe bronchus. It was removed, together with much necrotic, mucoid debris. On microscopic examination, the “foreign body” was necrotic, containing large numbers of hyphae and conidia in a manner typical of an aspegilloma or fungal cast. The culture grew A.fumigatus.
Clinical and radiologic improvement followed bronchoscopy, and itraconazole therapy was begun because of the concern about invasive aspergillosis in the setting of marked neutropenia. The patient tolerated the medication well at a dose of 200 mg twice daily, and the chest film became normal over the subsequent six weeks, after which itraconazole was discontinued. A sputum specimen cultured for fungus four weeks after the start of therapy was negative. After the initial improvement with itraconazole, the patient had recurrent urosepsis, associated with dehydration and marked confusion. Nine weeks after the discontinuation of itraconazole, he died of progressive dementia complicated by recurrent pneumonia and sepsis. There was no postmortem examination.
This patient was described (pt 11) and this chest radiograph reproduced in Denning DW, Follansbee S, Scolaro M, Norris S, Edelstein D, Stevens DA. Pulmonary Aspergillosis in the Acquired Immunodeficiency Syndrome. N Engl J Med 1991; 324: 654-662.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
Image A. Scan shows large bore needle in one of the cavities on the right. The contrast media is mixed with amphotericin B and is whiter than surrounding lung tissue and fungal ball. The contrast surrounds the aspergilloma present in this cavity. Some of the contrast has fallen by gravity in another cavity anteriorly below the one being injected, showing communication between the cavities.
Image B. Scan showing contrast media mixed with amphotericin B injected into a multicystic cavity in the right upper lobe. The contrast (white) flows around the aspergilloma present in this cavity. The contrast falls by gravity posteriorly.
Image C. The opposite lung shows multiple empty cystic spaces with little normal lung.
Image D. There is substantial pleural thickening surrounding the irregular cavity containing the aspergilloma.
 ,
,  ,
,  ,
, 
-
Extensive multilobar, varicose bronchiectasis, with some cyst formation most marked on the left anteriorly. Also some inhomogeneity of the pulmonary parenchyma secondary to air trapping in several affected segments.
-
CT scans of thorax. Anterior left-sided bronchiectasis with extensive mucous plugging and with some proximal bronchiectasis and plugging on the right.

-
Bilateral multilobar varicose bronchiectasis affecting the segmental and small order bronchi, with some distal plugging.
-
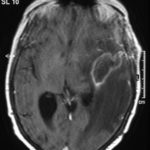
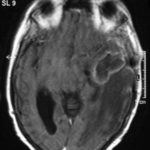
T1 weighted, gadolinium enhanced magnetic resonance brain scan. This 43 year-old alcoholic woman underwent laparoscopic cholecystectomy in January 2001. Ten days after surgery, she became confused, dysphasic and eventually had tonic-clonic seizures. A CT scan showed non-communicating hydrocephalus with ventriculitis. She underwent many complicated neurosurgical interventions, and received long term broad-spectrum antimicrobials and dexamethasone. One month later, she had generalized seizures, and a large abscess was observed on scan (see images). A heavy growth of A. fumigatus was retrieved from the abscess, and amphotericin B and 5-flucytosine were started. Antifungal therapy was changed voriconazole due to intolerance to amphotericin B and worsening disorientation. Voriconazole dosing (which varied from 300mg to 100mg twice daily) was guided by plasma concentrations as enzyme induction with rifampicin and carbamazepine, and reduction in clearance with alcoholic liver disease complicated her voriconazole dosing. Steroids were gradually reduced. She had a good recovery and completed 9 months of voriconazole.
Despite air filtration in the operating rooms, she apparently acquired an intra-operative infection, probably accelerated in presentation by concurrent dexamethasone. Rapid diagnosis and optimization of voriconazole dosing lead to a good outcome.
 ,
,  ,
,  ,
,  ,
,  ,
, 
-
Allergic Broncho-pulmonary aspergillosis. Pt CT. Extensive severe saccular bronchiectasis of the left lower lobe and to a lesser extent of the left upper and right lower lobe.
-
Ct scan of chest. This patient with severe ABPA, serologically and radiologically, developed a spectrum of lesions in the lung. In this cut, a cavitating infiltrate in the anterior segment of the left upper lobe was visualised together with some bronchial thickening and bronchiectasis in the left upper and lower lobe.




 ,
,  ,
,  ,
, 
 ,
,  ,
,  ,
,