Date: 26 November 2013
The patient was a 37-year old man in whom P.carinii pneumonia developed in August 1987, followed by esophageal candidiasis and upper gastrointestinal bleeding in September. Chronic perineal herpes led to the formation of rectourethral fistula and multiple episodes of urosepsis, for which he was given long-term ciprofloxacin therapy to suppress bacterial colonization of the bladder. He discontinued heavy alcohol use in September 1987 and smoked marijuana occasionally.On April 23 1989, the patient was admitted to the hospital with a two-month history of increasing dry cough with shortness of breath. He reported transient fever (temperature to 41°C). He was admitted with leukopenia, with his neutrophil count falling to 16 x 106/l on the second hospital day. A chest film showed bilateral fluffy lower-lobe infiltrates (this image). Zidovudine was discontinued. The patient had a rapidly downhill course despite intravenous treatment with trimethioprim-sulfamethoxazole. A bronchoscopy on the sixth hospital day revealed what appeared to be a foreign body in the left lower-lobe bronchus. It was removed, together with much necrotic, mucoid debris. On microscopic examination, the “foreign body” was necrotic, containing large numbers of hyphae and conidia in a manner typical of an aspegilloma or fungal cast. The culture grew A.fumigatus.
Clinical and radiologic improvement followed bronchoscopy, and itraconazole therapy was begun because of the concern about invasive aspergillosis in the setting of marked neutropenia. The patient tolerated the medication well at a dose of 200 mg twice daily, and the chest film became normal over the subsequent six weeks, after which itraconazole was discontinued. A sputum specimen cultured for fungus four weeks after the start of therapy was negative. After the initial improvement with itraconazole, the patient had recurrent urosepsis, associated with dehydration and marked confusion. Nine weeks after the discontinuation of itraconazole, he died of progressive dementia complicated by recurrent pneumonia and sepsis. There was no postmortem examination.
This patient was described (pt 11) and this chest radiograph reproduced in Denning DW, Follansbee S, Scolaro M, Norris S, Edelstein D, Stevens DA. Pulmonary Aspergillosis in the Acquired Immunodeficiency Syndrome. N Engl J Med 1991; 324: 654-662.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
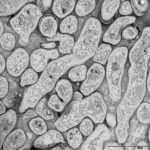
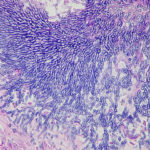
Light microscopic image of hyphae in an aspergilloma (10x magnification)

-
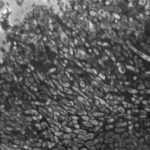
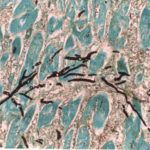
Light microscopic image of hyphae in an aspergilloma (400x magnification)
-
An aspergilloma (or fungal ball) is a mass of fungus found inside the body, for example inside cavities such as the lungs or sinuses, or as abscesses in organs such as the brain or kidney. They are made up of threadlike fungal strands (hyphae) that are densely packed but only around 1/200 of a millimetre in diameter. A mass of hyphae is called a mycelium.
In this image, a slice through an aspergilloma has been imaged using a transmission electron microscope.
-
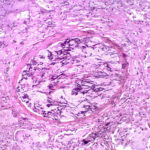
Aspergillus can punch through the lining of the lungs and invade the blood vessels below, in a process called angioinvasion. It can result in blockage (occlusion) of the blood vessel and damage to the local tissue through lack of oxygen (infarction). In severely immunocompromised patients, fragments can even break off and travel to other organs in the body.
In this image, a tissue section through a blocked blood vessel has been stained with the dyes haematoxylin (purple, binds DNA) and eosin (pink, binds proteins).
-
Showing the edge of a colony of aspergillus forming a fungal ball. The fungal hyphae exhibit dichotomous 45 degree angle branching and septae typical of Aspergillus.
-
Pt CJ finger clubbing, this patient had chronic cavitary pulmonary aspergillosis, with an aspergilloma since 1988, following an episode of haemoptysis. Currently patient still has symptomatic disease.
Images E,F Blood stained sputum samples from this patient.
 ,
,  ,
,  ,
,  ,
,  ,
, 
-
Disseminated, invasive aspergillosis showing dichotomously branching hyphae. Original magnification x300. Stained with Gomori Methenamine Silver (GMS).
-
Disseminated, invasive aspergillosis showing dichotomously branching hyphae. Original magnification x150. Stained with Gomori Methenamine Silver (GMS).

-
Disseminated, invasive aspergillosis showing dichotomously branching hyphae. Original magnification x50. Stained with Gomori Methenamine Silver (GMS).

-
Light microscopical appearance of invasive pulmonary aspergillosis showing vessel occlusion with thrombus and distal infarction (Haematoxylin and eosin, x100)