Date: 26 November 2013
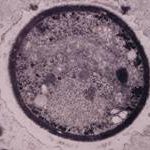
The patient was a 37-year old man in whom P.carinii pneumonia developed in August 1987, followed by esophageal candidiasis and upper gastrointestinal bleeding in September. Chronic perineal herpes led to the formation of rectourethral fistula and multiple episodes of urosepsis, for which he was given long-term ciprofloxacin therapy to suppress bacterial colonization of the bladder. He discontinued heavy alcohol use in September 1987 and smoked marijuana occasionally.On April 23 1989, the patient was admitted to the hospital with a two-month history of increasing dry cough with shortness of breath. He reported transient fever (temperature to 41°C). He was admitted with leukopenia, with his neutrophil count falling to 16 x 106/l on the second hospital day. A chest film showed bilateral fluffy lower-lobe infiltrates (this image). Zidovudine was discontinued. The patient had a rapidly downhill course despite intravenous treatment with trimethioprim-sulfamethoxazole. A bronchoscopy on the sixth hospital day revealed what appeared to be a foreign body in the left lower-lobe bronchus. It was removed, together with much necrotic, mucoid debris. On microscopic examination, the “foreign body” was necrotic, containing large numbers of hyphae and conidia in a manner typical of an aspegilloma or fungal cast. The culture grew A.fumigatus.
Clinical and radiologic improvement followed bronchoscopy, and itraconazole therapy was begun because of the concern about invasive aspergillosis in the setting of marked neutropenia. The patient tolerated the medication well at a dose of 200 mg twice daily, and the chest film became normal over the subsequent six weeks, after which itraconazole was discontinued. A sputum specimen cultured for fungus four weeks after the start of therapy was negative. After the initial improvement with itraconazole, the patient had recurrent urosepsis, associated with dehydration and marked confusion. Nine weeks after the discontinuation of itraconazole, he died of progressive dementia complicated by recurrent pneumonia and sepsis. There was no postmortem examination.
This patient was described (pt 11) and this chest radiograph reproduced in Denning DW, Follansbee S, Scolaro M, Norris S, Edelstein D, Stevens DA. Pulmonary Aspergillosis in the Acquired Immunodeficiency Syndrome. N Engl J Med 1991; 324: 654-662.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
BAL specimen showing hyaline, septate hyphae consistent with Aspergillus, stained with Blankophor
-
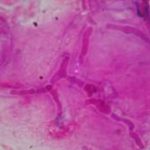
Mucous plug examined by light microscopy with KOH, showing a network of hyaline branching hyphae typical of Aspergillus, from a patient with ABPA.

-
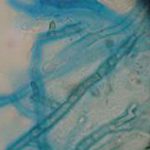
Corneal scraping stained with lactophenol cotton blue showing beaded septate hyphae not typical of either Fusarium spp or Aspergillus spp, being more consistent with a dematiceous (ie brown coloured) fungus
-
Corneal scrape with lactophenol cotton blue shows separate hyphae with Fusarium spp or Aspergillus spp.
-
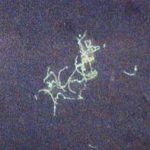
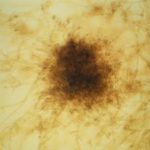
A filamentous fungus in the CSF of a patient with meningitis that grew Candida albicans in culture subsequently.
-
Transmission electron micrograph of a C. neoformans cell seen in CSF in an AIDS patients with remarkably little capsule present. These cells may be mistaken for lymphocytes.
-
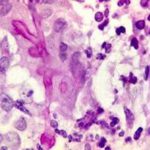
India ink preparation of CSF showing multiple yeasts with large capsules, and narrow buds to smaller daughter cells, typical of C. neoformans