Date: 26 November 2013
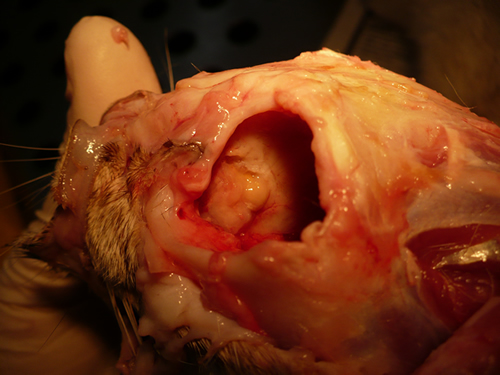
Nasal, sinus and orbital aspergillosis in a cat. The left nasal cavity and sinus were full of pus and debris and there was severe bone erosion from the nasal cavity into the rostromedial orbitthrough which pus was protruding
Copyright:
(Kindly provided by Martin L. Whitehead, BSc, PhD, BVSc, CertSAM, MRCVS & Peter W. Kettlewell, BVSc, MSc, MRCVS. Chipping Norton Veterinary Hospital, Albion Street, Chipping Norton, Oxon, OX7 5BN.)
Notes:
History : Nasal aspergillosis is relatively common in dogs but rare in cats. Our veterinary hospital in Oxfordshire was recently presented with a 13-year old female Burmilla cat with a history of left-side unilateral nasal discharge, a watery left eye with slight blepharospasm, occasional ‘twitching movements’ of the head, weight loss, inappetance and depression. Clinical examination was unremarkable except for left-side mucopurulent nasal discharge, left-side mild serous ocular discharge, and a soft subcutaneous swelling over the left frontal sinus. Haematology, blood biochemistry and urinalysis revealed diabetes mellitus but was otherwise unremarkable. Radiography under general anaesthesia revealed a diffuse soft tissue density within the left nasal cavity and left frontal sinus. Rhinoscopy revealed mucopurulent discharge on the left side but was otherwise unremarkable. Aspiration of the swelling over the left frontal sinus produced pus and this abscess was lanced and flushed. The frontal sinus was trephined and the sinus and nasal cavity flushed with saline. Tests for feline immunodeficiency virus and feline leukaemia virus and serology for Aspergillus were not carried out. The cat was started on insulin, ibafloxacin (Ibaflin, Intervet) and meloxicam (Metacam, Boehringer). Cytology of the material flushed from the frontal sinus and nasal cavity revealed fungal hyphae consistent with Aspergillus species and culture of this material yielded growth of a fungus which was morphologically similar to A. candidus (Awaiting molecular typing results). The cat was then started on oral itraconazole (Itrafungol, Janssen) 10 mg/kg p.o. SID. The abscess over the rostral frontal sinus did not heal and a second abscess appeared over the nasal bone just dorsal to the nose. Infusion of the frontal sinus and nasal cavity with topical antifungal medication was discussed with the owners, but as the cat was deteriorating they requested euthanasia. On post-mortem examination the right nasal cavity, frontal sinus and orbit were unaffected. The left nasal cavity and sinus were full of pus and debris and there was severe bone erosion from the nasal cavity into the rostromedial orbit through which pus was protruding. There was also severe bone erosion rostrally through the nasal bone and less severe bone erosion dorsally over the rostral part of the frontal sinus, these sites of bone erosion being at the location of the two subcutaneous abscesses.Feline nasal aspergillosis is extremely rare in the UK and to our knowledge this is the first reported case of orbital aspergillosis in the UK although nasal aspergillosis has been reported in other countries.
Images library
-
Title
Legend
-
A Colonies on MEA after one week, B conidial head x920, C atypical reduced conidial head x920, D conidial head x 920.

-
A case of onychomycosis associated with Aspergillus ochraceopetaliformis as described in Med Mycol. 2009 Mar 9:1-5, 2009,Brasch J, Varga J, Jensen JM, Egberts F & Tintelnot K

-
Histology of the infected nail (PAS stain) showing thick fungal elements and septate hyphae within nail material.
-
culture and identified in a case of onychomycosis – Culture at higher magnification.
-
culture and identified in a case of onychomycosis – Culture of Aspergillus ochraceopetaliformis on Sabouraud agar with cycloheximide at 26C

-
This patient with chronic cavitary pulmonary aspergillosis was treated with itraconazole, with some success, but considerable gastrointestinal disturbance (diarrhoea, flatulence and uncomfortable feeling in his abdomen). He also developed a facial rash. Itraconazole was stopped and he reverted to voriconazole which he was unable to take because of a severe feeling of being generally unwell. His facial rash resolved. Application was made for funding posaconazole. He started this and after 6 weeks an almost identical facial rash to that seen with itraconazole appeared. He tolerated posaconazole well in other respects, and his chronic cavitary pulmonary aspergillosis is now significantly better (symptomatically and serologically). July 2007
 ,
,  ,
,  ,
, 
-
This patient with ABPA and chronic cavitary pulmonary aspergillosis has been stabilized on voriconazole treatment for >5 years. She had a degree of photosensitivity most of that time, noticed early in the course of voriconazole treatment. She is oxygen and wheelchair dependent and doesn’t go outside very much, so most of her light exposure has been indoor light. She developed rough scaly patches over her face, neck and lower arms. Dermatological review indicated multiple solar keratoses”. Skin biopsy from the right forearm confirmed this clinical diagnosis – “skin showing hyperkeratosis with a little parakeratosis and acanthosis. The keratinocytes have a glassy appearance but show nuclear atypia with dyskeratotic cells, and occasional suprabasal mitoses. The intraepidermal sweat ducts are spared. Appearances suggest an actinic keratosis with moderate to severe dysplasia.” These features are characteristic of a low grade premalignant change.
She was treated with local 5-fluorouracil cream (Efudix) (3 cycles) to the affected lesions. These photos were taken at the apogee of inflammation. The inflammation resolved after discontinuing the cream. This reaction is expected with application of this mild chemotherapy agent. Alternative or supplementary treatments include cryotherapy, curettage and cautery, if necessary. Following treatment her skin was much softer and considerably improved. Voriconazole has been stopped, and posaconazole substituted.
 ,
,  ,
,  ,
,