Date: 7 February 2014
Image B
Copyright:
Dr D Denning, Wythenshawe Hospital, Manchester.(© Fungal Infection Trust)
Notes:
Images library
-
Title
Legend
-
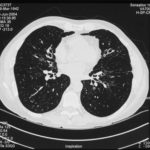
High resolution CT scan images with reconstruction of 1mm thick slices at approximately 10mm increments. The scan shows moderately severe multi-lobar cylindrical and varicose bronchiectasis predominantly centrally and in the upper lungs. There is no mucus plugging seen.
The features are in keeping with allergic bronchopulmonary aspergillosis
 ,
,  ,
, 
-
pt.SB – 6/10/98 – bronchocentric granulomatosis. CT scan showing multiple small nodules of variable size in both lung fields, apparently close to the vascular bundles.

-
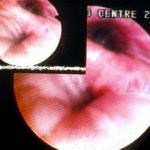
Bronchial oedema.Remarkably oedematous bronchial mucosa, as seen in ABPA.
-
An example of longstanding allergic bronchopulmonary aspergillosis in a patient who has been steroid dependent for over 15 years showing remarkable kyphoscoliosis and honey combing and fibrosis of both lungs.

-
Recurrent pulmonary shadows 1. 6 Jan 1988 – chest radiograph showing right hilar enlargement, consistent with ABPA.
Recurrent pulmonary shadows 1. 3 Feb 1989 – chest radiograph showing right upper-lobe consolidation and contraction consistent with obstruction of RUL bronchus, in ABPA.
Clearing of pulmonary shadows 3, pt BJ. 5 April 1989 – resolution of shadows seen in February, with a course of corticosteroids.
Recurrence of pulmonary shadows 4, pt BJ. 2 September 1989 – recurrence of pulmonary shadows with an exacerbation of ABPA.
Central bronchiectasis, pt BJ. CT scan of thorax October 1989 showing central bronchiectasis, characteristic of ABPA (and cystic fibrosis).
 ,
,  ,
,  ,
,  ,
, 
-
A typical example of a wet mount of a sputum sample from a patient with allergic bronchopulmonary aspergillosis.