Date: 26 November 2013
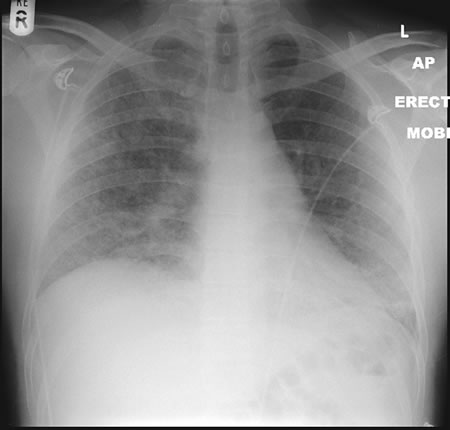
22/09/08 This chest radiograph shows bilateral hazy diffuse airspace disease predominating in the lower lungs with subtle nodularity in upper zones.
Copyright: n/a
Notes:
A 33 year old known Chronic Granulomatous Disorder (CGD) male presented to A&E in respiratory distress and admitted with severe bibasal pneumonia. He had been laying mulch in his garden. He had not been taking any prophylactic antifungal agents. Oxygen therapy was commenced in conjunction with IV bacterial and fungal treatment with Amphotericin B (Fungizone ®). Further consultation and an adverse reaction to the administration of Fungizone ® led to a switch to IV Voriconazole 300mg BD. The patient tested positive for aspergillus antibodies in serum. The patient declined a bronchoscopy, responded well to IV voriconazole and was discharged home 2 weeks post admission on maintenance voriconazole.
Images library
-
Title
Legend
-
This patient with ABPA and chronic cavitary pulmonary aspergillosis has been stabilized on voriconazole treatment for >5 years. She had a degree of photosensitivity most of that time, noticed early in the course of voriconazole treatment. She is oxygen and wheelchair dependent and doesn’t go outside very much, so most of her light exposure has been indoor light. She developed rough scaly patches over her face, neck and lower arms. Dermatological review indicated multiple solar keratoses”. Skin biopsy from the right forearm confirmed this clinical diagnosis – “skin showing hyperkeratosis with a little parakeratosis and acanthosis. The keratinocytes have a glassy appearance but show nuclear atypia with dyskeratotic cells, and occasional suprabasal mitoses. The intraepidermal sweat ducts are spared. Appearances suggest an actinic keratosis with moderate to severe dysplasia.” These features are characteristic of a low grade premalignant change.
She was treated with local 5-fluorouracil cream (Efudix) (3 cycles) to the affected lesions. These photos were taken at the apogee of inflammation. The inflammation resolved after discontinuing the cream. This reaction is expected with application of this mild chemotherapy agent. Alternative or supplementary treatments include cryotherapy, curettage and cautery, if necessary. Following treatment her skin was much softer and considerably improved. Voriconazole has been stopped, and posaconazole substituted.
 ,
,  ,
,  ,
, 
-
Patient NG -ocular redness and erythema due to voriconazole.