Date: 26 November 2013
Patient MD with kyphoscoliosis and chronic cavitary pulmonary aspergillosis and an aspergilloma. Patient exhibited azole resistant A. fumigatus.
Further details
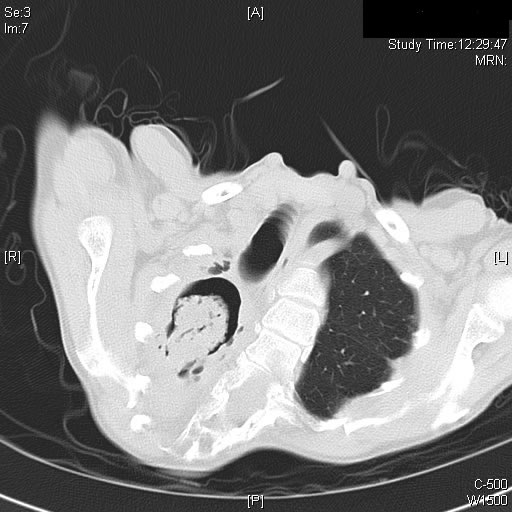
Image A. This CT scan cut shown shows a grossly distorted thorax because of the kyphoscoliosis, a nearly normal appearing left lung, her trachea at an odd angle, demonstrating the normal cartilage rings and an aspergilloma in a cavity which has replaced the right upper lobe. The cavity is surrounded by significant pleural thickening and fibrosis.
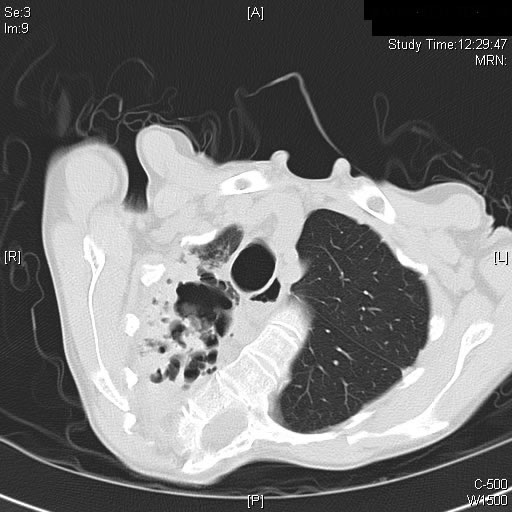
Image B. The other cut (slightly inferior) shows a complex large cavity and some smaller ones posteriorly, with some material consistent with a fungal ball within the large cavity. There is a separate cavity anteriorly and small air spaces within the extensive pleural thickening. Her trachea is widened. the left lung appears normal.
This patient with repaired juvenile scoliosis first recognised that she had pulmonary aspergillosis when she coughed up large amounts of blood, she was admitted to ICU and underwent bronchial artery embolisation, followed by tranexamic acid orally. A. fumigatus was cultured from sputum. A diagnosis of chronic cavitary pulmonary aspergillosis with an aspergilloma was made. She didn’t improve with itraconazole (no fall in Aspergillus precipitins and continuing symptoms, despite good blood levels) and was treated with voriconazole. She had a good sympomatic response, with marginal improvement in her Aspergillus precipitins titre. Remission continued for over 3 years but then her symptoms of cough and general fatigue returned. Her sputum grew A. fumigatus again, which had MICs to itraconazole (>8 mg/L, resistant), voriconazole (8mg/L, resistant) and posaconazole (2mg/mL, resistant). She is being treated with amphotericin B.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
Image A
CT Scan 30/3/99
Showing extreme pleural thickening and 2 small cavities at apex of left lung.
-
A 43 year old with smoking related emphysema was admitted to hospital with two separate episodes of haemoptysis. He had been in good health up to 1989, when he was diagnosed as having bilateral pulmonary tuberculosis. At that time a CT scan revealed a cavity in the left upper lobe (20.8cm2) with adjacent confluent infiltrates and pleural thickening. On bronchoscopic examination no abnormalities were noted and endobronchial biopsies did not reveal hyphae.
Over the next 4 years his condition deteriorated and a CT scan showed the left upper lobe cavity had increased to 40cm2. Itraconazole 400mg daily was prescribed. There was some clinical improvement on itraconazole but patient eventually deteriorated with breathlessness and with significant weight loss.
 ,
,