Date: 26 November 2013
This recording of peak flow was taken prior to and during the first 4 weeks of inhaled steroids (Becotide 100 and Duovent both 2 puffs 4x daily). The patient had had asthma since age 4, and been treated with bronchodilators and oral courses of steroids when severely affected. The chart, which the patient completed at home, shows that early in week one her peak flow varied from 200-250 L/min. As the medication started to work, the peak flows gradually increased to reach 360-420 L/min in the 4th week. The lower value each morning is characteristic of asthma.
The response to steroids is important confirmation of the diagnosis of asthma (reversible airways obstruction). Many years later she developed ABPA, while on inhaled steroids, with severe upper lobe central bronchiectasis, an IgE of 6,800 Kiu/L, positive aspergillus precipitins, an Aspergillus RAST of 58.7KUa/L (normal <0.4) and eosinophilia.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
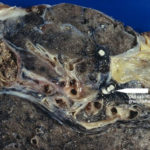
Macroscopic view medial aspect of left upper lobe of lung showing segmental collapse and congestion of lower segments, with mucus extruding from incised bronchi.
 ,
,  ,
,  ,
,  ,
, 
-
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.