Date: 26 November 2013
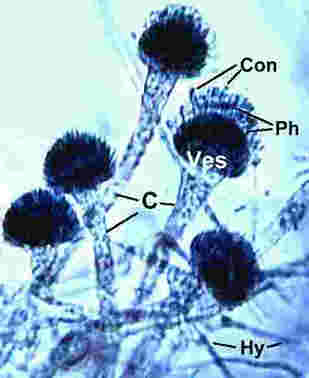
microscopic characters Conidiophore stipes(C)225-350um arising from hyphae(Hy):Vesicles(Ves)15-25um wide:Phialides(Ph)uniseriate:Conidia(Con)2.4-3.0um spherical to ovoid,roughened.
Copyright:
Fungal Research Trust
Notes:
Colonies on CYA 40-60 mm diam, plane or lightly wrinkled, low, dense and velutinous or with a sparse, floccose overgrowth; mycelium inconspicuous, white; conidial heads borne in a continuous, densely packed layer, Greyish Turquoise to Dark Turquoise (24-25E-F5); clear exudate sometimes produced in small amounts; reverse pale or greenish. Colonies on MEA 40-60 mm diam, similar to those on CYA but less dense and with conidia in duller colours (24-25E-F3); reverse uncoloured or greyish. Colonies on G25N less than 10 mm diam, sometimes only germination, of white mycelium. No growth at 5°C. At 37°C, colonies covering the available area, i.e. a whole Petri dish in 2 days from a single point inoculum, of similar appearance to those on CYA at 25°C, but with conidial columns longer and conidia darker, greenish grey to pure grey.
Conidiophores borne from surface hyphae, stipes 200-400 µm long, sometimes sinuous, with colourless, thin, smooth walls, enlarging gradually into pyriform vesicles; vesicles 20-30 µm diam, fertile over half or more of the enlarged area, bearing phialides only, the lateral ones characteristically bent so that the tips are approximately parallel to the stipe axis; phialides crowded, 6-8 µm long; conidia spherical to subspheroidal, 2.5-3.0 µm diam, with finely roughened or spinose walls, forming radiate heads at first, then well defined columns of conidia.
Distinctive features
This distinctive species can be recognised in the unopened Petri dish by its broad, velutinous, bluish colonies bearing characteristic, well defined columns of conidia. Growth at 37°C is exceptionally rapid. Conidial heads are also diagnostic: pyriform vesicles bear crowded phialides which bend to be roughly parallel to the stipe axis. Care should be exercised in handling cultures of this species.
Images library
-
Title
Legend
-
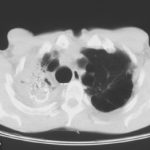
Image A. Scan shows large bore needle in one of the cavities on the right. The contrast media is mixed with amphotericin B and is whiter than surrounding lung tissue and fungal ball. The contrast surrounds the aspergilloma present in this cavity. Some of the contrast has fallen by gravity in another cavity anteriorly below the one being injected, showing communication between the cavities.
Image B. Scan showing contrast media mixed with amphotericin B injected into a multicystic cavity in the right upper lobe. The contrast (white) flows around the aspergilloma present in this cavity. The contrast falls by gravity posteriorly.
Image C. The opposite lung shows multiple empty cystic spaces with little normal lung.
Image D. There is substantial pleural thickening surrounding the irregular cavity containing the aspergilloma.
 ,
,  ,
,  ,
, 
-
Extensive multilobar, varicose bronchiectasis, with some cyst formation most marked on the left anteriorly. Also some inhomogeneity of the pulmonary parenchyma secondary to air trapping in several affected segments.
-
CT scans of thorax. Anterior left-sided bronchiectasis with extensive mucous plugging and with some proximal bronchiectasis and plugging on the right.

-
Bilateral multilobar varicose bronchiectasis affecting the segmental and small order bronchi, with some distal plugging.
-
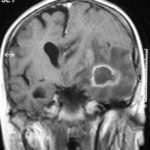
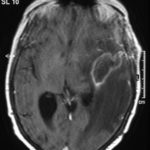
T1 weighted, gadolinium enhanced magnetic resonance brain scan. This 43 year-old alcoholic woman underwent laparoscopic cholecystectomy in January 2001. Ten days after surgery, she became confused, dysphasic and eventually had tonic-clonic seizures. A CT scan showed non-communicating hydrocephalus with ventriculitis. She underwent many complicated neurosurgical interventions, and received long term broad-spectrum antimicrobials and dexamethasone. One month later, she had generalized seizures, and a large abscess was observed on scan (see images). A heavy growth of A. fumigatus was retrieved from the abscess, and amphotericin B and 5-flucytosine were started. Antifungal therapy was changed voriconazole due to intolerance to amphotericin B and worsening disorientation. Voriconazole dosing (which varied from 300mg to 100mg twice daily) was guided by plasma concentrations as enzyme induction with rifampicin and carbamazepine, and reduction in clearance with alcoholic liver disease complicated her voriconazole dosing. Steroids were gradually reduced. She had a good recovery and completed 9 months of voriconazole.
Despite air filtration in the operating rooms, she apparently acquired an intra-operative infection, probably accelerated in presentation by concurrent dexamethasone. Rapid diagnosis and optimization of voriconazole dosing lead to a good outcome.
 ,
,  ,
,  ,
,  ,
,  ,
, 
-
Allergic Broncho-pulmonary aspergillosis. Pt CT. Extensive severe saccular bronchiectasis of the left lower lobe and to a lesser extent of the left upper and right lower lobe.
-
Ct scan of chest. This patient with severe ABPA, serologically and radiologically, developed a spectrum of lesions in the lung. In this cut, a cavitating infiltrate in the anterior segment of the left upper lobe was visualised together with some bronchial thickening and bronchiectasis in the left upper and lower lobe.


 ,
,  ,
,  ,
, 
 ,
,  ,
,  ,
,