Date: 7 May 2013
Copyright: n/a
Notes:
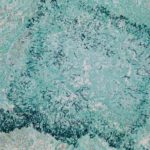
Colonies on CYA 40-60 mm diam, plane or lightly wrinkled, low, dense and velutinous or with a sparse, floccose overgrowth; mycelium inconspicuous, white; conidial heads borne in a continuous, densely packed layer, Greyish Turquoise to Dark Turquoise (24-25E-F5); clear exudate sometimes produced in small amounts; reverse pale or greenish. Colonies on MEA 40-60 mm diam, similar to those on CYA but less dense and with conidia in duller colours (24-25E-F3); reverse uncoloured or greyish. Colonies on G25N less than 10 mm diam, sometimes only germination, of white mycelium. No growth at 5°C. At 37°C, colonies covering the available area, i.e. a whole Petri dish in 2 days from a single point inoculum, of similar appearance to those on CYA at 25°C, but with conidial columns longer and conidia darker, greenish grey to pure grey.
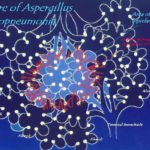
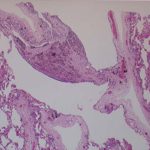
Conidiophores borne from surface hyphae, stipes 200-400 µm long, sometimes sinuous, with colourless, thin, smooth walls, enlarging gradually into pyriform vesicles; vesicles 20-30 µm diam, fertile over half or more of the enlarged area, bearing phialides only, the lateral ones characteristically bent so that the tips are approximately parallel to the stipe axis; phialides crowded, 6-8 µm long; conidia spherical to subspheroidal, 2.5-3.0 µm diam, with finely roughened or spinose walls, forming radiate heads at first, then well defined columns of conidia.
Distinctive features
This distinctive species can be recognised in the unopened Petri dish by its broad, velutinous, bluish colonies bearing characteristic, well defined columns of conidia. Growth at 37°C is exceptionally rapid. Conidial heads are also diagnostic: pyriform vesicles bear crowded phialides which bend to be roughly parallel to the stipe axis. Care should be exercised in handling cultures of this species.
Images library
-
Title
Legend
-
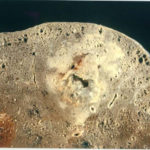
Pt MW Chronic Pulmonary Aspergillosis An example of bloody, thick, sputum from a patient with a destroyed left lung containing 2 large cavities, each with an aspergilloma.
 ,
, 
-
Further details
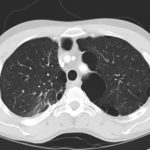
June 2009 – CT scan of the chest (two images D & E). These scans show residual large bullae, particularly notable in the apex of the left lung on both cuts. Small residual bullae remain in the right apex following a bullectomy which greatly reduced the size and number of these lesions.
Pt RK Lung bullae caused by cannabis smoking complicated by pneumothorax and chronic cavitary pulmonary aspergillosis.
February 2009 – Chest x-ray showing bilateral apical bullae most marked on the right in association with a right pneumothorax. A chest drain is in-situ.
Late February 2009 – persistent apical bullae right upper zone with resolving pneumothorax. Chest drain still in-situ. Increasing right upper lobe shadowing possibly representing infection or haemorrhage.
April 2009 – Post-operative chest x-ray showing post apical bullectomy on the right, resolved pneumothorax but the interval development of fluid in the right costo-phrenic angle with air fluid levels consistent with recent surgery. Great reduction in apical bullae in the right apex but increasing consolidation proximally in the right upper zone and some fluid in the horizontal fissure. These findings are following an apical bullectomy and pleurodesis of his prior significant pneumothorax.
June 2009 – CT scan of the chest (two images – see above). These scans show residual large bullae, particularly notable in the apex of the left lung on both cuts. Small residual bullae remain in the right apex following a bullectomy which greatly reduced the size and number of these lesions.
This patient underwent a bullectomy to remove part of the lung after developing lung bullae associated with cannabis smoking. The transverse section (G) of the specimen clearly shows the bullae along the left side and lower edge of the section. I and J demonstrate the dark pigment seen in accumulated macrophages. Tobacco smoking alone also causes a dark pigment, but evidence suggests that in marijuana smokers this pigment accumulates much faster and even with reduced exposure. The manner in which marijuana is smoked ie. without a filter and extended holding of the breath may contribute to this observation.
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
, 
-
History
Since March 2004, this 49 year old atopic lady has developed end-stage lung disease following a long history of severe steroid dependant asthma with recurrent infective exacerbations and colonisations by Aspergillus fumigatus and Pseudomonas aeruginosa. Both organisms had been isolated from sputum and previously an Aspergillus precipitins test was positive with an elevated total IgE level. Despite initial treatment with oral Itraconazole, chest X-rays were supportive of gross cystic bronchiectatic cavities in both apices and on CT scan a right upper lobe mycetoma (fungal ball). A diagnosis of allergic broncho-pulmonary Aspergillosis ABPA, with radiological evidence of bilateral apical fibrosis, was continuously treated with antifungal and Colomycin Nebulisers. This lady’s disease continued to deteriorate she developed Type 2 respiratory failure and was established on long term oxygen therapy (LTOT) of 2l/min via an oxygen concentrator at home and oxygen conserver when mobile. No recognised benefit was gained from a trial of non-invasive ventilation therapy and DEXA scan confirmed steroid induced osteoporosis resulting in a right sided rib fracture. Increasingly difficult venous access led to the insertion of a right sub-clavian Portocath for administration of intravenous antibiotic therapy. Systemic steroids, nebulisers and long term antifungal therapies did not prevent disease progression of ABPA to chronic cavitatory Aspergillosis.
She has been treated with voriconazole with some benefit, but slow deterioration, so that she is now 4l/min oxygen dependent 24 hours a day.

-
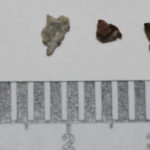
This man with chronic cavitary pulmonary aspergillosis, has been on continuous antifungal therapy for 4 years, initially itraconazole (with intracavity amphotericin B), then a short course of amphotericin B, then voriconazole with a period of interferon gamma, now posaconazole. He is co-infected with Mycobacterium xenopi, and has chronically abnormal liver function tests, of uncertain aetiology. Previously he coughed up plug-like material, and recently black hard material that is completely solid. This occurred following a 4 month period of sustained improvement on posaconazole (aspergillus precipitin titre has fallen from 1/32 to positive undiluted), but with relapsing M. xenopi infection
 ,
,  ,
, 

![Asp[1]fumighead2copyr Asp[1]fumighead2copyr](https://www.aspergillus.org.uk/wp-content/uploads/2013/11/Asp1fumighead2copyr.jpg)