Date: 7 May 2013
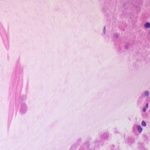
A four day A. fumigatus culture on malt extract agar (above). Light microscopy pictures are taken at 1000x mag., stained with lacto-phenol cotton blue (right).
Copyright:
With thanks to Niall Hamilton.
Notes:
Colonies on CYA 40-60 mm diam, plane or lightly wrinkled, low, dense and velutinous or with a sparse, floccose overgrowth; mycelium inconspicuous, white; conidial heads borne in a continuous, densely packed layer, Greyish Turquoise to Dark Turquoise (24-25E-F5); clear exudate sometimes produced in small amounts; reverse pale or greenish. Colonies on MEA 40-60 mm diam, similar to those on CYA but less dense and with conidia in duller colours (24-25E-F3); reverse uncoloured or greyish. Colonies on G25N less than 10 mm diam, sometimes only germination, of white mycelium. No growth at 5°C. At 37°C, colonies covering the available area, i.e. a whole Petri dish in 2 days from a single point inoculum, of similar appearance to those on CYA at 25°C, but with conidial columns longer and conidia darker, greenish grey to pure grey.
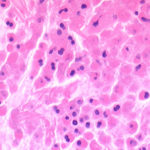
Conidiophores borne from surface hyphae, stipes 200-400 µm long, sometimes sinuous, with colourless, thin, smooth walls, enlarging gradually into pyriform vesicles; vesicles 20-30 µm diam, fertile over half or more of the enlarged area, bearing phialides only, the lateral ones characteristically bent so that the tips are approximately parallel to the stipe axis; phialides crowded, 6-8 µm long; conidia spherical to subspheroidal, 2.5-3.0 µm diam, with finely roughened or spinose walls, forming radiate heads at first, then well defined columns of conidia.
Distinctive features
This distinctive species can be recognised in the unopened Petri dish by its broad, velutinous, bluish colonies bearing characteristic, well defined columns of conidia. Growth at 37°C is exceptionally rapid. Conidial heads are also diagnostic: pyriform vesicles bear crowded phialides which bend to be roughly parallel to the stipe axis. Care should be exercised in handling cultures of this species.
Images library
-
Title
Legend
-
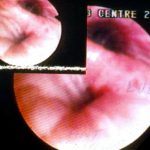
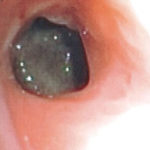
A. Necrotic mass prolapsing in and out of the distal right intermediate bronchus obscuring both the basal stem and basal division

-
History : A 20 yr old female with cystic fibrosis complicated by CF-related Diabetes mellitus (diagnosed at age 12 years) & ABPA (diagnosed at
15 years ). She was fairly stable until last 9 months, when she started to experience frequent pulmonary exacerbations, which have prompted intensive therapies.
Her serum IgE at the time of diagnosis was 5060 IU/L, skin prick test for aspergillus was positive, and serum was positive for precipitating antibodies to Aspergillus. She was treated with oral prednisone (1 mg/kg/day) for first two weeks followed by prednisone at 0.5 mg/kg every other day for at least 6 months with some clinical and serologic improvement. Over the following 5 years, she presented with a pattern of repeated episodic exacerbations with wheezing and crackles, increases in IgE and need to increase prednisone dosage. In an attempt to control her frequent ABPA relapses, itraconazole was added at 200mg twice a day, with some clinical & serologic improvement.
2-3 weeks prior to the scans and X rays, she developed severe protracted coughing spells associated with minor hemoptysis, low grade intermittent fever, and weight loss. Her FEV1 declined in a 3 months period from 56% to 33%.
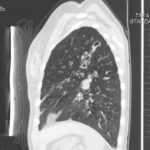
A chest-x ray (Fig 3) did not reveal any new changes when compared to the one obtained almost a year before. A CT scan of the chest Figs 1 and 2- lateral view), however shows an ovoid soft tissue density within an ectatic bronchi in the anterior basal segment of the LLL, felt to be an aspergilloma.She was started on oral voriconazole (3 months after the above scans and X-rays) which is better absorbed in CF patients than itraconazole, at 200mg twice a day. Her prednisone was gradually reduced to 5 mgs/day and her FEV1 increased to 46% of predicted (03/31/10), her IgE level was 1167 kU/L (previously in January 2009, her IgE level was 3053 kU/L)and her weight has plateaued.
Since she was not fit enough for surgery at that time, removing the aspergilloma by flexible bronchoscopy was unsuccessful. The aspergilloma can be seen at bronchoscopy in Fig 4. ,
,  ,
,  ,
, 
-
Widespread mucoid impaction also seen, particularly in left side, suggestive of allergic bronchopulmonary aspergillosis.

-
Microscopy of fungal hyphae isolated from fungal culture (lactophenol blue)
-
A CT scan performed at this time showed an enhancing lesion with ill defined margins involving the pterigopalatine fossa, the maxillary antrum , orbital apex and middle cranial fossa. There was also destruction of boney architecture locally.
-
The patient underwent a pneumonectomy because of the severity of her disease process, and uncertainty about the diagnosis, prior to serology results being obtained.
Serology showed an IgE of 2600, with a strongly positive Aspergillus RAST test and weakly positive Aspergillus precipitins. Material removed at bronchoscopy showed eosinophilia. These features confirm a diagnosis of allergic bronchopulmonary aspergillosis (ABPA).
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
, 

![Asp[1]fumighead Asp[1]fumighead](https://www.aspergillus.org.uk/wp-content/uploads/2013/11/Asp1fumighead.jpg)

 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,