Date: 26 November 2013
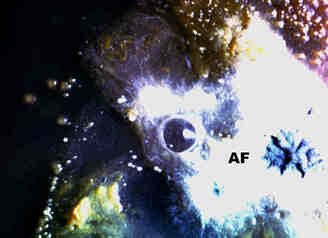
Plugs cultured on agarA young colony of the fungus(AF) has a central patch of sporulation and is surrounded by colonies of bacteria and yeasts.
Copyright: n/a
Notes:
Colonies on CYA 40-60 mm diam, plane or lightly wrinkled, low, dense and velutinous or with a sparse, floccose overgrowth; mycelium inconspicuous, white; conidial heads borne in a continuous, densely packed layer, Greyish Turquoise to Dark Turquoise (24-25E-F5); clear exudate sometimes produced in small amounts; reverse pale or greenish. Colonies on MEA 40-60 mm diam, similar to those on CYA but less dense and with conidia in duller colours (24-25E-F3); reverse uncoloured or greyish. Colonies on G25N less than 10 mm diam, sometimes only germination, of white mycelium. No growth at 5°C. At 37°C, colonies covering the available area, i.e. a whole Petri dish in 2 days from a single point inoculum, of similar appearance to those on CYA at 25°C, but with conidial columns longer and conidia darker, greenish grey to pure grey.
Conidiophores borne from surface hyphae, stipes 200-400 µm long, sometimes sinuous, with colourless, thin, smooth walls, enlarging gradually into pyriform vesicles; vesicles 20-30 µm diam, fertile over half or more of the enlarged area, bearing phialides only, the lateral ones characteristically bent so that the tips are approximately parallel to the stipe axis; phialides crowded, 6-8 µm long; conidia spherical to subspheroidal, 2.5-3.0 µm diam, with finely roughened or spinose walls, forming radiate heads at first, then well defined columns of conidia.
Distinctive features
This distinctive species can be recognised in the unopened Petri dish by its broad, velutinous, bluish colonies bearing characteristic, well defined columns of conidia. Growth at 37°C is exceptionally rapid. Conidial heads are also diagnostic: pyriform vesicles bear crowded phialides which bend to be roughly parallel to the stipe axis. Care should be exercised in handling cultures of this species.
Images library
-
Title
Legend
-
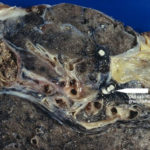
Macroscopic view medial aspect of left upper lobe of lung showing segmental collapse and congestion of lower segments, with mucus extruding from incised bronchi.
 ,
,  ,
,  ,
,  ,
, 
-
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.