Date: 26 November 2013
Aspergillus flavus
Copyright:
© Fungal Research Trust
Notes:
Colonies on CYA 60-70 mm diam, plane, sparse to moderately dense, velutinous in marginal areas at least, often floccose centrally, sometimes deeply so; mycelium only conspicuous in floccose areas, white; conidial heads usually borne uniformly over the whole colony, but sparse or absent in areas of floccose growth or sclerotial production, characteristically Greyish Green to Olive Yellow (1-2B-E5-7), but sometimes pure Yellow (2-3A7-8), becoming greenish in age; sclerotia produced by about 50% of isolates, at first white, becoming deep reddish brown, density varying from inconspicuous to dominating colony appearance and almost entirely suppressing conidial production; exudate sometimes produced, clear, or reddish brown near sclerotia; reverse uncoloured or brown to reddish brown beneath sclerotia. Colonies on MEA 50-70 mm diam, similar to those on CYA although usually less dense. Colonies on G25N 25-40 mm diam, similar to those on CYA or more deeply floccose and with little conidial production, reverse pale to orange or salmon. No growth at 5°C. At 37°C, colonies usually 55-65 mm diam, similar to those on CYA at 25°C, but more velutinous, with olive conidia, and sometimes with more abundant sclerotia.
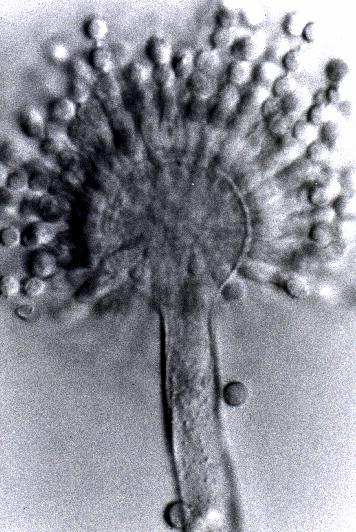
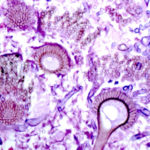
Sclerotia produced by some isolates, at first white, rapidly becoming hard and reddish brown to black, spherical, usually 400- 800 µm diam. Teleomorph not known. Conidiophores borne from subsurface or surface hyphae, stipes 400 µm to 1 mm or more long, colourless or pale brown, rough walled; vesicles spherical, 20-45 µm diam, fertile over three quarters of the surface, typically bearing both metulae and phialides, but in some isolates a proportion or even a majority of heads with phialides alone; metulae and phialides of similar size, 7-10 µm long; conidia spherical to subspheroidal, usually 3.5-5.0 µm diam, with relatively thin walls, finely roughened or, rarely, smooth.
Distinctive features
Aspergillus flavus is distinguished by rapid growth at both 25°C and 37°C, and a bright yellow green (or less commonly yellow) conidial colour. A. flavus produces conidia which are rather variable in shape and size, have relatively thin walls, and range from smooth to moderately rough, the majority being finely rough.
Images library
-
Title
Legend
-
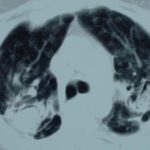
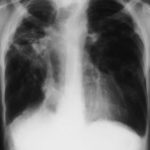
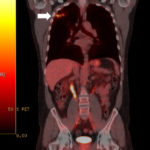
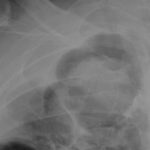
This 54 year old man developed right upper lobe shadowing after development of cough, chest pain and shortness of breath. He suffered from emphysema. Investigations, including a PET scan suggested carcinoma of the lung. He underwent an apical resection and histology showed bullae in the lung with one containing necrotic material and conidial heads consistent with Aspergillus.
Histology:
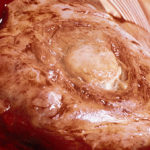
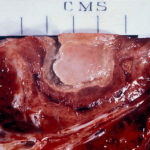
Two wedges of lung tissue were examined. The larger 90 x 35 x 35mm with adherent parietal pleura 100 x 45mm. Sectioning reveals irregular scarring and bullae in the lung tissue. No definite tumour is identified. A focus of possible necrosis up to 10mm in diameter is present, 10mm from the pleura and 20mm from the nearest staple line. Lung and adherent parietal pleura show dense fibrosis around a cavity (see fig A) arrow, lined by granulation tissue and fibrin. This is filled with necrotic material (Fig B) and branching septate fungal hyphae with conidial heads, consistent with Aspergillus and a fungal ball.(Fig C at higher power). A few scattered granulomata are seen away from the cavity. No invasion of lung parenchyma was seen. There is congestion of the lung parenchyma and collections of pigmented macrophages are seen within air spaces.Legends:
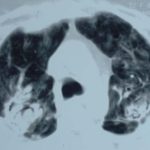
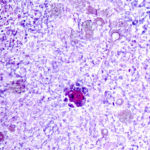
A- Section of lung showing a fungal ball within a cavity (x25). B- Showing branching septate hyphae with conidial heads (x250) C- Higher power magnification (x 500) showing the conidial heads more clearly. D – Edge of cavity showing from left to right – necrosis, granulaomatous reaction, fibrosis, chronic inflammation (x100). E- CT scan (July 08) showing a speculated nodular lesion in the right apex. F – Chest X-ray (May 08) – showing right upper lobe shadowing. G.PET scan (July 08)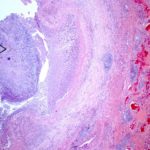 ,
,  ,
,  ,
,  ,
,  ,
,  ,
, 
-
Pt DB This patient with longstanding pulmonary disease developed Mycobacterium avium pulmonary infection which was treated. X rays in Jan 05 through to May 06 revealed an aspergilloma in upper right lobe cavity. Following a severe prolonged bout of coughing up black material- X rays on 22/9/07 showed a disappearance of the aspergilloma.( Images G & H). Go to case history
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
, 
-
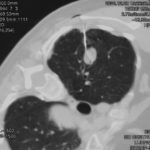
This 63 year old smoker presented with a new small mass in the right upper lobe. She had had tuberculosis as a teenager (1958) which recurred in 1962, requiring 2 long stays in a sanatorium. Since then she was well, until a new shadow was noticed on her chest X-ray. A CT showed a smooth round nodule, and to rule out carcinoma it was biopsied percutaneously. Histology showed fungal hyphae, consistent with Aspergillus , and serology confirmed infection with Aspergillus fumigatus. Following biopsy, an air fluid pocket has appeared, most consistent with an aspergilloma, as the lesion is solitary.
-
Patient MD with kyphoscoliosis and chronic cavitary pulmonary aspergillosis and an aspergilloma. Patient exhibited azole resistant A. fumigatus.
Further details
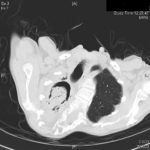
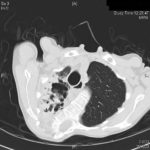
Image A. This CT scan cut shown shows a grossly distorted thorax because of the kyphoscoliosis, a nearly normal appearing left lung, her trachea at an odd angle, demonstrating the normal cartilage rings and an aspergilloma in a cavity which has replaced the right upper lobe. The cavity is surrounded by significant pleural thickening and fibrosis.
Image B. The other cut (slightly inferior) shows a complex large cavity and some smaller ones posteriorly, with some material consistent with a fungal ball within the large cavity. There is a separate cavity anteriorly and small air spaces within the extensive pleural thickening. Her trachea is widened. the left lung appears normal.
This patient with repaired juvenile scoliosis first recognised that she had pulmonary aspergillosis when she coughed up large amounts of blood, she was admitted to ICU and underwent bronchial artery embolisation, followed by tranexamic acid orally. A. fumigatus was cultured from sputum. A diagnosis of chronic cavitary pulmonary aspergillosis with an aspergilloma was made. She didn’t improve with itraconazole (no fall in Aspergillus precipitins and continuing symptoms, despite good blood levels) and was treated with voriconazole. She had a good sympomatic response, with marginal improvement in her Aspergillus precipitins titre. Remission continued for over 3 years but then her symptoms of cough and general fatigue returned. Her sputum grew A. fumigatus again, which had MICs to itraconazole (>8 mg/L, resistant), voriconazole (8mg/L, resistant) and posaconazole (2mg/mL, resistant). She is being treated with amphotericin B.
 ,
, 
-
Histopathological appearance of a fungus ball: it consists of a tangled mass of branching, septate hyphal with vesicular swellings in the center (H&E, x 200).

-
Further image details
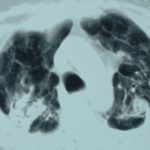
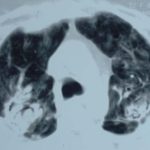
Image A. Long standing sarcoidosis, on corticosteroids with fibrosis and cavitary disease, and a possible fungal ball in the cavity on the left (1996).
Image B. Long standing sarcoidosis, on corticosteroids with 2 cavities containing aspergillomas, one on the left and one on the right (1996).
Image C. Sarcoidosis with progressive cavity formation and aspergillomas. Probable CIPA given appearances (2000).
Image D. Sarcoidosis with progressive cavity formation and aspergillomas. Probable CIPA given appearances (2000).
Image E. Sarcoidosis with progressive cavity formation and aspergillomas. Probable CIPA given appearances (2000).
 ,
,  ,
,  ,
,  ,
,