Date: 26 November 2013
cultures grown from BAL fluid showing formation of sclerotia.
Copyright:
Kindly donated by Dr Claudia Venturelli and Dr Giorgia Bertazzoni, Laboratory of Microbiology – Policlinico of Modena-Italy. © Fungal Research Trust
Notes:
These colonies were isolated from a BAL, (also with bacterial qrowth of S.aureus and S.maltophilia) from a patient with a VAP (undergoing corticosteroid treatment). The growth medium used is sabouraud dextrose agar , incubated at 37° C The identification is made by microscopic/macroscopic observation criteria.
Colonies on CYA 60-70 mm diam, plane, sparse to moderately dense, velutinous in marginal areas at least, often floccose centrally, sometimes deeply so; mycelium only conspicuous in floccose areas, white; conidial heads usually borne uniformly over the whole colony, but sparse or absent in areas of floccose growth or sclerotial production, characteristically Greyish Green to Olive Yellow (1-2B-E5-7), but sometimes pure Yellow (2-3A7-8), becoming greenish in age; sclerotia produced by about 50% of isolates, at first white, becoming deep reddish brown, density varying from inconspicuous to dominating colony appearance and almost entirely suppressing conidial production; exudate sometimes produced, clear, or reddish brown near sclerotia; reverse uncoloured or brown to reddish brown beneath sclerotia. Colonies on MEA 50-70 mm diam, similar to those on CYA although usually less dense. Colonies on G25N 25-40 mm diam, similar to those on CYA or more deeply floccose and with little conidial production, reverse pale to orange or salmon. No growth at 5°C. At 37°C, colonies usually 55-65 mm diam, similar to those on CYA at 25°C, but more velutinous, with olive conidia, and sometimes with more abundant sclerotia.
Sclerotia produced by some isolates, at first white, rapidly becoming hard and reddish brown to black, spherical, usually 400- 800 µm diam. Teleomorph not known. Conidiophores borne from subsurface or surface hyphae, stipes 400 µm to 1 mm or more long, colourless or pale brown, rough walled; vesicles spherical, 20-45 µm diam, fertile over three quarters of the surface, typically bearing both metulae and phialides, but in some isolates a proportion or even a majority of heads with phialides alone; metulae and phialides of similar size, 7-10 µm long; conidia spherical to subspheroidal, usually 3.5-5.0 µm diam, with relatively thin walls, finely roughened or, rarely, smooth.
Distinctive features
Aspergillus flavus is distinguished by rapid growth at both 25°C and 37°C, and a bright yellow green (or less commonly yellow) conidial colour. A. flavus produces conidia which are rather variable in shape and size, have relatively thin walls, and range from smooth to moderately rough, the majority being finely rough.
Images library
-
Title
Legend
-
5 sputum samples were positive for A. niger, a bronchoscopy was normal and culture and microscopy were negative. Rx voriconazole, 200mg bd was given. An excellent clinical response was seen.
 ,
,  ,
,  ,
,  ,
, 
-
The patient was a 37-year old man in whom P.carinii pneumonia developed in August 1987, followed by esophageal candidiasis and upper gastrointestinal bleeding in September. Chronic perineal herpes led to the formation of rectourethral fistula and multiple episodes of urosepsis, for which he was given long-term ciprofloxacin therapy to suppress bacterial colonization of the bladder. He discontinued heavy alcohol use in September 1987 and smoked marijuana occasionally.On April 23 1989, the patient was admitted to the hospital with a two-month history of increasing dry cough with shortness of breath. He reported transient fever (temperature to 41°C). He was admitted with leukopenia, with his neutrophil count falling to 16 x 106/l on the second hospital day. A chest film showed bilateral fluffy lower-lobe infiltrates (this image). Zidovudine was discontinued. The patient had a rapidly downhill course despite intravenous treatment with trimethioprim-sulfamethoxazole. A bronchoscopy on the sixth hospital day revealed what appeared to be a foreign body in the left lower-lobe bronchus. It was removed, together with much necrotic, mucoid debris. On microscopic examination, the “foreign body” was necrotic, containing large numbers of hyphae and conidia in a manner typical of an aspegilloma or fungal cast. The culture grew A.fumigatus.
Clinical and radiologic improvement followed bronchoscopy, and itraconazole therapy was begun because of the concern about invasive aspergillosis in the setting of marked neutropenia. The patient tolerated the medication well at a dose of 200 mg twice daily, and the chest film became normal over the subsequent six weeks, after which itraconazole was discontinued. A sputum specimen cultured for fungus four weeks after the start of therapy was negative. After the initial improvement with itraconazole, the patient had recurrent urosepsis, associated with dehydration and marked confusion. Nine weeks after the discontinuation of itraconazole, he died of progressive dementia complicated by recurrent pneumonia and sepsis. There was no postmortem examination.
This patient was described (pt 11) and this chest radiograph reproduced in Denning DW, Follansbee S, Scolaro M, Norris S, Edelstein D, Stevens DA. Pulmonary Aspergillosis in the Acquired Immunodeficiency Syndrome. N Engl J Med 1991; 324: 654-662.
 ,
, 
-
Image A. This 25 year old woman was previously well and presented with a pneumonia of uncertain aetiology. She has infiltrates in right upper-lobe and left middle and lower zones. The diagnosis was later made of chronic invasive pulmonary aspergillosis by bronchoscopy . Subsequently she was diagnosed with adult-onset chronic granulomatous disease with neutrophil function assays.
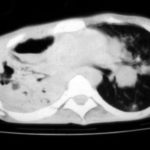
Image B. CT scan of the thorax just below the carina, showing almost complete opacification of the right lung and marked nodular shadowing around the hilum of the left lung.
Image C. Progression of pulmonary infiltrates are seen seven weeks later, despite administration of amphotericin B.
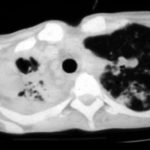
Image D. CT scan of the thorax above the carina showing near complete opacification of the right lung and multiple discrete nodular shadows in the left lung.
 ,
,  ,
,  ,
, 
-
02/10/09 X -ray shows improvement in appearances from initial presentation with complete chest radiographic resolution by 07/11/2008

-
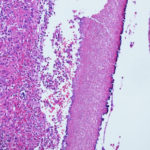
Subacute IPA in rhematoid nodules of the lung. in a patient with rheumatoid arthritis. Histology sections stained with H&E