Date: 26 November 2013
History : A 20 yr old female with cystic fibrosis complicated by CF-related Diabetes mellitus (diagnosed at age 12 years) & ABPA (diagnosed at
15 years ). She was fairly stable until last 9 months, when she started to experience frequent pulmonary exacerbations, which have prompted intensive therapies.
Her serum IgE at the time of diagnosis was 5060 IU/L, skin prick test for aspergillus was positive, and serum was positive for precipitating antibodies to Aspergillus. She was treated with oral prednisone (1 mg/kg/day) for first two weeks followed by prednisone at 0.5 mg/kg every other day for at least 6 months with some clinical and serologic improvement. Over the following 5 years, she presented with a pattern of repeated episodic exacerbations with wheezing and crackles, increases in IgE and need to increase prednisone dosage. In an attempt to control her frequent ABPA relapses, itraconazole was added at 200mg twice a day, with some clinical & serologic improvement.
2-3 weeks prior to the scans and X rays, she developed severe protracted coughing spells associated with minor hemoptysis, low grade intermittent fever, and weight loss. Her FEV1 declined in a 3 months period from 56% to 33%.
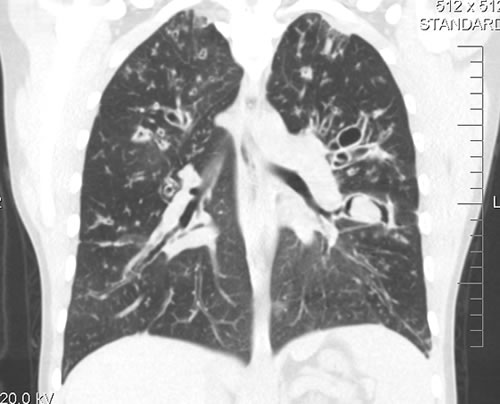
A chest-x ray (Fig 3) did not reveal any new changes when compared to the one obtained almost a year before. A CT scan of the chest Figs 1 and 2- lateral view), however shows an ovoid soft tissue density within an ectatic bronchi in the anterior basal segment of the LLL, felt to be an aspergilloma.
She was started on oral voriconazole (3 months after the above scans and X-rays) which is better absorbed in CF patients than itraconazole, at 200mg twice a day. Her prednisone was gradually reduced to 5 mgs/day and her FEV1 increased to 46% of predicted (03/31/10), her IgE level was 1167 kU/L (previously in January 2009, her IgE level was 3053 kU/L)and her weight has plateaued.
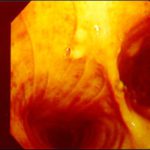
Since she was not fit enough for surgery at that time, removing the aspergilloma by flexible bronchoscopy was unsuccessful. The aspergilloma can be seen at bronchoscopy in Fig 4.
Go to follow up 12 months later
Copyright:
Kindly donated by Dr N Turcios, Director of pediatric pulmonology/cystic fibrosis in Somerville, NJ.
Notes: n/a
Images library
-
Title
Legend
-
This 24-year-old male with AML on chemotherapy developed recent onset fever and cough. B- Representative section of High Resolution CT shows centri-lobular nodules, ‘tree-in-bud’ appearance consistent with bronchogenic spread of disease.

-
This 24-year-old male with AML on chemotherapy developed recent onset fever and cough. A: Chest radiograph showing patchy air space consolidation involving both lungs.

-
This man with severe chronic fibrosing alveolitis underwent a single left lung transplant at the end of November 2004. Postoperatively he developed reperfusion pulmonary oedema and was difficult to ventilate. He also developed acute renal failure requiring haemodialysis/haemofiltration which corrected his fluid overload and rising creatinine.Rejection was prevented with cyclosporin, mycophenolate and a decreasing dose of methylprednisolone. Cardiovascular problems identified mild pulmonary anastomostic stenosis with a 5% pressure gradient. He had a tracheostomy about 12 days post transplant. He then developed episodes of hypoxia and increased ventilatory pressures. Several bronchoscopies showed mucus plugging in the trachea and major bronchi. These were aspirated, with improvement of oxygenation. Cultures of one of these plugs grew A. fumigatus. These images show a bronchoscopy view of the trachea and anastomosis. Major obstruction of the airway is visible (70%) distal to the anastomosis which looks healthy. Some evidence of tracheal inflammation is visible.
 ,
, 
-
The chest x-ray shows a patient who had a left lung transplanted in May 2003 for cryptogenic fibrosing alveolitis, which was diagnosed post-transplant as sarcoidosis.

-
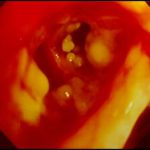
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.

-
Tracheal aspergillosis, Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.

-
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.
-
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.
-
Aspergillus tracheobronchitis in a normal child. This figure, drawn in 1890, illustrates the appearances of the trachea and main bronchi at autopsy in a 3 year old child. She had little else wrong at autopsy other than a minor degree of tuberculosis. She is the first recorded case of Aspergillus tracheobronchitis in the literature and illustrates well that this disease can affect previously well non-inimmunocompromised people. The full case is reported in Wheaton SW.

-
pt FT. Normal chest radiograph of patient with extensive pseudomembranous Aspergillus tracheobronchitis, 4 days before death.