Date: 26 November 2013
History : A 20 yr old female with cystic fibrosis complicated by CF-related Diabetes mellitus (diagnosed at age 12 years) & ABPA (diagnosed at
15 years ). She was fairly stable until last 9 months, when she started to experience frequent pulmonary exacerbations, which have prompted intensive therapies.
Her serum IgE at the time of diagnosis was 5060 IU/L, skin prick test for aspergillus was positive, and serum was positive for precipitating antibodies to Aspergillus. She was treated with oral prednisone (1 mg/kg/day) for first two weeks followed by prednisone at 0.5 mg/kg every other day for at least 6 months with some clinical and serologic improvement. Over the following 5 years, she presented with a pattern of repeated episodic exacerbations with wheezing and crackles, increases in IgE and need to increase prednisone dosage. In an attempt to control her frequent ABPA relapses, itraconazole was added at 200mg twice a day, with some clinical & serologic improvement.
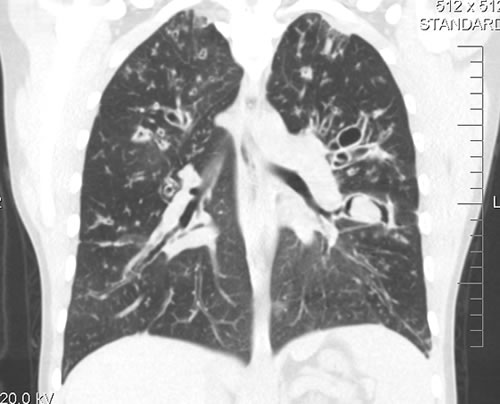
2-3 weeks prior to the scans and X rays, she developed severe protracted coughing spells associated with minor hemoptysis, low grade intermittent fever, and weight loss. Her FEV1 declined in a 3 months period from 56% to 33%.
A chest-x ray (Fig 3) did not reveal any new changes when compared to the one obtained almost a year before. A CT scan of the chest Figs 1 and 2- lateral view), however shows an ovoid soft tissue density within an ectatic bronchi in the anterior basal segment of the LLL, felt to be an aspergilloma.
She was started on oral voriconazole (3 months after the above scans and X-rays) which is better absorbed in CF patients than itraconazole, at 200mg twice a day. Her prednisone was gradually reduced to 5 mgs/day and her FEV1 increased to 46% of predicted (03/31/10), her IgE level was 1167 kU/L (previously in January 2009, her IgE level was 3053 kU/L)and her weight has plateaued.
Since she was not fit enough for surgery at that time, removing the aspergilloma by flexible bronchoscopy was unsuccessful. The aspergilloma can be seen at bronchoscopy in Fig 4.
Go to follow up 12 months later
Copyright:
Kindly donated by Dr N Turcios, Director of pediatric pulmonology/cystic fibrosis in Somerville, NJ.
Notes: n/a
Images library
-
Title
Legend
-
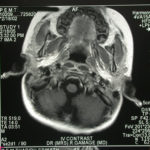
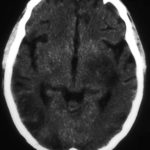
Image a. 3 yr old boy with CNS aspergillosis pt TS. MRI scan pre-amphotericin B
-
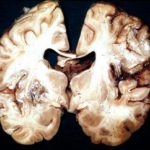
Section though unfixed brain showing large pale area of infarction deep in the parietal cortex, in which Aspergillus hyphae were seen histologically. The patient developed disseminated aspergillosis after a prolonged stay in intensive care after contracting severe community acquired pneumonia.
-
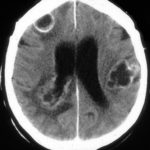
The woman had received a renal transplant several months prior to developing a stroke with reduced consciousness. The enhanced CT scan of her brain showed multiple ring-enhancing lesions bilaterally with little surrounding oedema. Biopsy confirmed invasive aspergillosis on histology and culture.
-
Further details
Image A. Multiple ring enhancing abscesses with substantial surrounding oedema was demonstrated. He had no focal neurological deficits. A needle aspiration confirmed the clinical impression of cerebral aspergillosis by culture and microscopy.
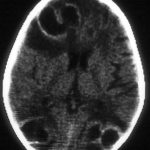
Image B. Resolution of cerebral aspergillosis, pt MN. Focal scars with some surrounding oedema are seen in the site of the prior abscesses.
 ,
, 
-
Contrast enhanced CT scan of the brain showing unequivocally 2 hypodense lesions, one in the left basal ganglia and one in the right occipital cortex. There is the possibility of another smaller left sided occiptal cortex. These lesions do not have the appearance of abscesses, but rather of ischaema.

-
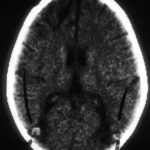
Unenhanced CT scan of the brain in an allogeneic bone marrow transplant recipient demonstrating a large, variably hypodense lesion in the area of the left basal ganglia and possible additional lesions in the posterior parietal and/or occipital cortex.
-
A. versicolor by microscopy showing very long thin conidiophores.

-
Pigmentation of Aspergillus versicolor colonies ranged from pale green to greenish-beige, pink-green, dark green and brown. Reverse is usually reddish. The growth rate is usually slow. Cultured on Sabouraud dextrose agar with chloramphenicol.

-
A Colonies on MEA after one week; B, C conidial heads with tip of conidiophire, x920; D conidial head, x 2330; E conidial heads x920

-
Cultures were grown on malt extract agar. Image kindly provided by Niall Hamilton.