Date: 26 November 2013
X-Rays -Allergic Bronchopulmonary Aspergillosis (ABPA) with 3 relapses.
A female patient JO (50 yrs) with right middle lobe collapse. The patient presented with a 6 month history of cough which has persisted despite antibiotics and both steroid and salbutamol inhalers. She then developed acute breathlessness with coughing and wheezing. There was no history of asthma. Bronchoscopy (Image K) showed a mucous plug obstructing the right upper lobe bronchus.
Images D – G are X rays showing relapse in 1998 and recovery
Images H – J are X rays showing relapse in 2003
Image K. Bronchoscopy appearance of mucous impaction of the bronchus intermedius – pt JO (50yrs). There was a long mucous plug in the anterior segment of the RUL. Half of this was aspirated and sent for microscopy and culture. The second half “fell into” the bronchus intermedius (which feeds the right middle lobe) and was only partially aspirated.
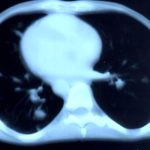
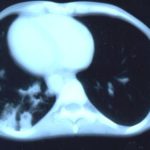
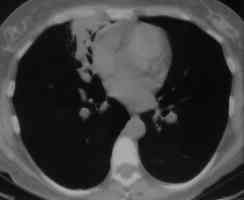
Images L – O: High resolution CT scan of thorax in pt JO, post bronchoscopy. 1.5mm sections at 1 cm intervals of whole lung. There is collapse and consolidation in the right middle lobe with dilation of the right middle lobe bronchi. There is also minor bronchiectasis in the right upperlobe with a little patchy air space shadowing . There is no mediastinal lymphadenopathy or any interstitial fibrosis.
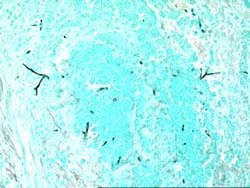
Image P & Q: Histology: Mucous plug (3x 0.5x 0.5cm) containing numerous inflammatory cells, including eosinophils and nuclear debris.GMS staining reveals occasional fungal hyphae with septa and dichotomous branching. These appearances support the diagnosis of bronchopulmonary Aspergillosis. Bronchioalveolar lavage fluid was negative on microscopy and no fungi were grown. A year later Aspergillus fumigatus was grown from her sputum.
Copyright: n/a
Notes: n/a
Images library
-
Title
Legend
-
Pt AR Interval development of chronic cavitary pulmonary aspergillosis in the context of sarcoidosis
This patient was diagnosed with sarcoid after developing a chronic cough with the attached chest X-ray. In February 2003 the X-ray demonstrated bilateral extensive changes consistent with fibrocystic sarcoidosis with a complex cavitary area in both apices, more marked on the right. She was given a course of corticosteroids.

-
Further details
Image B. Additional cavities are apparent inferior to this large cavity and are in communication both with the bronchi and the additional cavities. Some of the apparent cavities are probably dilated bronchi. The left lower lung is completely opacified otherwise. The degree of pleural fibrosis surrounding the left apical cavity is reduced slightly over the interval of four months.
Image C. This shows an almost normal hyperexpanded right lung with a very substantially contracted left lung with one large airway visible and probably incontinuity with a slightly irregular cavity containing some debris, presumably fungal tissue. Other levels show very large left apical cavity with numerous subsections containing debris or fibrotic tissue and almost complete fibrosis of the lung below the level of the carina on the left, with some calcification within the fibrotic lung tissue.
 ,
,  ,
, 
-
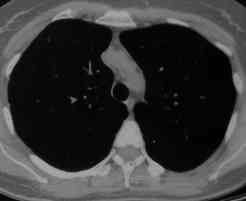
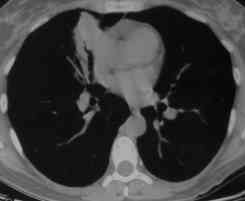
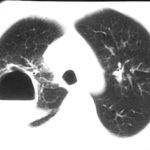
Transverse sections through the thorax of a patient with AIDS, hepatitis C and a left tempero-parietal cerebral lymphoma. His CD4 cell count was 45 x 106 / l. The lymphoma was proven by biopsy after a poor response to anti-toxoplasma therapy. He was given dexamethasone to cover the surgery and then developed diabetes mellitus. He did not receive chemotherapy for his lymphoma but did have 2 cerebral radiotherapy treatments (1.8 Gy each). Three weeks after the biopsy he developed dyspnoea and fever. Shortly after this he developed a right-sided hemiparesis, became comatose and died 2 days later.Autopsy showed a cerebral lymphoma and pulmonary and renal aspergillosis. Aspergillus nidulans was recovered from cultures of lungs and kidney.
 ,
,  ,
,  ,
, 
-
Fever chart of Pt CA -heart transplant pt with candidemia on amphotericin therapy, who developed pulmonary aspergillosis.

-
A Colonies on MEA + 20% sucrose after two weeks; B ascomata, x 40; C conidia and conidiophore, x 920; D ascospores and conidia x2330; E portion of ascoma with asci x920

-
A 66 yr old patient in good general health developed onychomycosis. Samples taken from the affected nail were grown by culture and examined by microscopy. Oral itraconazole pulse therapy was given to the patient (200 mg twice daily for 1 week, with 3 weeks off between successive pulses, for four pulses) and treatment was successful.
















 ,
,  ,
,  ,
,  ,
,  ,
, 
 ,
,  ,
, 