Date: 26 November 2013
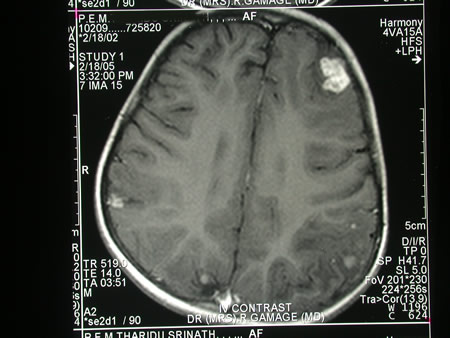
Image c. 3 yr old boy with CNS aspergillosis pt TS. MRI scan pre-amphotericin B
Copyright: n/a
Notes:
A 3 year old boy, quite active and healthy clinically, who has CNS aspergillosis. He was first seen about 4 months ago for a red eye, which turned out to be panophthalmitis; culture yielded Aspergillus spp. He received 2 weeks of iv amphotericin and was sent home by the ophthalmologists. No h/o eye trauma. He returned 2 weeks ago with focal fits, and the MR showed several lesions bilaterally (including ring enhancing lesions) and normal sinuses, and a brain bx showed fungal hyphae (no culture this time). His immune status (normal WCC and neutrophil function so far) was investigated.
He was given conventional amphotericin for 8 weeks, and switched to oral itraconazole. We had to limit the ampho to 0.7 mg/kg owing to toxicity (mainly hypokalaemia).
The MRI scan was repeated at about 6 weeks, and generally showed good improvement (scans e-h). The enhancement/flare were gone but remained in a few lesions, the lesions themselves were all either gone or much smaller. Further investigations revealed the child was immunocompetent.
Patient was switched from amphotericin to oral itraconazole at week 8 essentially on a clinical assessment. Awaiting follow-up.
Images library
-
Title
Legend
-
Macroscopic view medial aspect of left upper lobe of lung showing segmental collapse and congestion of lower segments, with mucus extruding from incised bronchi.
 ,
,  ,
,  ,
,  ,
, 
-
Born 75 years ago, Pt HK had 3 episodes of tuberculosis as a child and teenager, being treated with PAS and streptomycin. He suffered a ‘bad chest’ all his life and retired aged 54. Presenting with worsening and more frequent chest infections, he was referred with ‘bronchiectasis and Aspergillus sensitisation’. A diagnosis of chronic pulmonary aspergillosis was made in June 2009 on the basis of his chest radiograph and strongly positive Aspergillus precipitins (IgG antibodies) (titre 1/16). He also had Pseudomonas aeruginosa colonisation. His oxygen saturation was 87% and his pO2 6.8, pCO2 6.2 KPa.
His chest radiograph (see above, November 2009) was reported as showing; “ The lung fields are over-inflated. Bilateral apical fibrotic change secondary to old TB. No cavity seen.” At clinic, bilateral apical cavities were seen, with some associated pleural thickening at the left apex, without any evidence of a fungal ball.
He started posaconazole 400mg twice daily with therapeutic levels at subsequent visits. Sputum cultures never grew Aspergillus. Over the following 9 months he had no chest infections requiring antibiotics, his breathlessness worsened gradually and he remained easily fatigued. His Aspergillus antibody titres fell. Overall he felt better, but was concerned about declining respiratory status.