Date: 26 November 2013
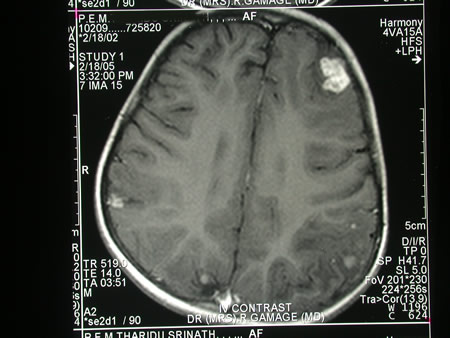
Image c. 3 yr old boy with CNS aspergillosis pt TS. MRI scan pre-amphotericin B
Copyright: n/a
Notes:
A 3 year old boy, quite active and healthy clinically, who has CNS aspergillosis. He was first seen about 4 months ago for a red eye, which turned out to be panophthalmitis; culture yielded Aspergillus spp. He received 2 weeks of iv amphotericin and was sent home by the ophthalmologists. No h/o eye trauma. He returned 2 weeks ago with focal fits, and the MR showed several lesions bilaterally (including ring enhancing lesions) and normal sinuses, and a brain bx showed fungal hyphae (no culture this time). His immune status (normal WCC and neutrophil function so far) was investigated.
He was given conventional amphotericin for 8 weeks, and switched to oral itraconazole. We had to limit the ampho to 0.7 mg/kg owing to toxicity (mainly hypokalaemia).
The MRI scan was repeated at about 6 weeks, and generally showed good improvement (scans e-h). The enhancement/flare were gone but remained in a few lesions, the lesions themselves were all either gone or much smaller. Further investigations revealed the child was immunocompetent.
Patient was switched from amphotericin to oral itraconazole at week 8 essentially on a clinical assessment. Awaiting follow-up.
Images library
-
Title
Legend
-
This 24-year-old male with AML on chemotherapy developed recent onset fever and cough. B- Representative section of High Resolution CT shows centri-lobular nodules, ‘tree-in-bud’ appearance consistent with bronchogenic spread of disease.

-
This 24-year-old male with AML on chemotherapy developed recent onset fever and cough. A: Chest radiograph showing patchy air space consolidation involving both lungs.

-
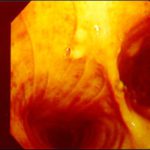
This man with severe chronic fibrosing alveolitis underwent a single left lung transplant at the end of November 2004. Postoperatively he developed reperfusion pulmonary oedema and was difficult to ventilate. He also developed acute renal failure requiring haemodialysis/haemofiltration which corrected his fluid overload and rising creatinine.Rejection was prevented with cyclosporin, mycophenolate and a decreasing dose of methylprednisolone. Cardiovascular problems identified mild pulmonary anastomostic stenosis with a 5% pressure gradient. He had a tracheostomy about 12 days post transplant. He then developed episodes of hypoxia and increased ventilatory pressures. Several bronchoscopies showed mucus plugging in the trachea and major bronchi. These were aspirated, with improvement of oxygenation. Cultures of one of these plugs grew A. fumigatus. These images show a bronchoscopy view of the trachea and anastomosis. Major obstruction of the airway is visible (70%) distal to the anastomosis which looks healthy. Some evidence of tracheal inflammation is visible.
 ,
, 
-
The chest x-ray shows a patient who had a left lung transplanted in May 2003 for cryptogenic fibrosing alveolitis, which was diagnosed post-transplant as sarcoidosis.

-
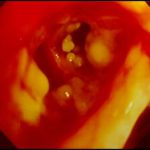
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.

-
Tracheal aspergillosis, Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.

-
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.
-
Tracheal aspergillosis. Bronchoscopic views of the trachea showing nodules in the trachea that revealed Aspergillus on biopsy. The patient had chronic lymphocytic leukaemia treated with fludarabine and corticosteroids and presented with wheezing and bilateral alveolar shadows.
-
Aspergillus tracheobronchitis in a normal child. This figure, drawn in 1890, illustrates the appearances of the trachea and main bronchi at autopsy in a 3 year old child. She had little else wrong at autopsy other than a minor degree of tuberculosis. She is the first recorded case of Aspergillus tracheobronchitis in the literature and illustrates well that this disease can affect previously well non-inimmunocompromised people. The full case is reported in Wheaton SW.

-
pt FT. Normal chest radiograph of patient with extensive pseudomembranous Aspergillus tracheobronchitis, 4 days before death.